Can a physical therapist bill Medicare for a progress report or discharge summary?
No, a physical therapist can not bill Medicare for a progress note. It is important you realize a progress note is not a physical therapy reevaluation. A progress report is not a separately payable event under Medicare Part B guidelines. A reevaluation is a separately payable event.
Note: A discharge summary is a type of progress report.
Related Article: CPT Code 97161 Physical Therapy Evaluation
How often does Medicare require a progress note for physical therapy?
10 Treatment Day Physical Therapy Progress Report Requirement
A progress report is required every 10 physical therapy treatment days (not calendar days) or sooner. If a physical therapist completes a progress report on the 7th treatment day then the next reporting period begins on treatment visit day number 8 and counts as the first of the next ten treatment day reporting period.
30 Day Requirement for PT Progress Reports
Medicare part B no longer requires a progress report to be completed every 30-days. That requirement ended in 2018.
Why physical therapists can’t bill Medicare for a progress report?
A physical therapy progress report is a requirement for reimbursement. It is not a separately payable event under the Medicare benefit policy manual.
Too many therapists are seeking reimbursement for a standard progress report because they are actually doing a physical therapy reevaluation and not a simple progress note.
A Progress Report is Not a Re-evaluation
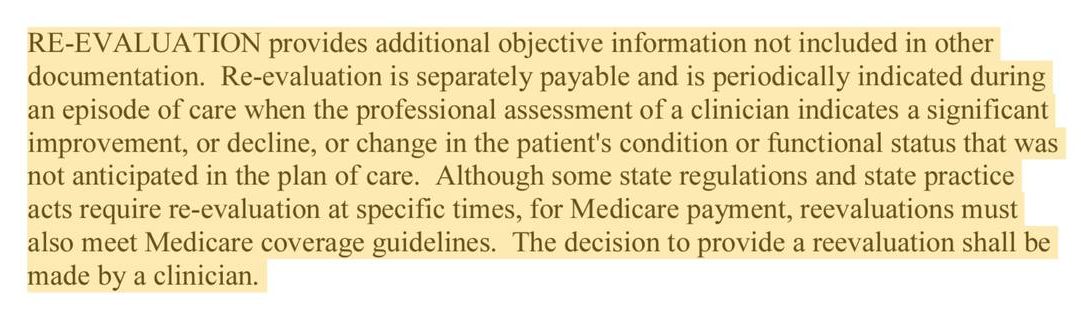
As you can see from the screenshot above, a Medicare re-evaluation is another evaluation. The most critical component in that definition is “not anticipated in the plan of care.”
Patients improve, plateau, and decline. All of those are anticipated. An example of something that is not expected is when you are treating a patient for hip pain attributed to osteoarthritis and then two weeks into a physical therapy plan of care, the patient receives an image report confirming a femur fracture.
In this case, a re-evaluation is warranted.
Does a referring physician need to sign a physical therapy progress report?
No, the referring physician or nonphysician practitioner does not need to sign a standard progress report.
For reference, this is what CMS Chapter 15 says on page 191 “It is not required that the referring or supervising physician/NPP sign the progress reports written by a PT, OT or SLP.”
When does a physician need to sign a progress report?
If your progress report is updating or changing the original plan of care it must be signed by the referring/certifying physician.
Examples include:
- when you are adding to the certification date range.
- when you are evaluating a new diagnosis and adding that diagnosis to the original plan of care.
- when you are making significant changes to the original plan of care.
What are the Medicare-required elements for a physical therapy progress report?
Based on CMS Chapter 15 Medicare Benefit Policy Manual page 194 a progress report requires the following elements:
- Date range of the reporting period. E.g. start date and end date.
- Date the report was written. Medicare states that a progress report may be completed up to 7 days after the reporting period ends.
- Signature, and professional identification, or for dictated documentation, the identification of the qualified professional who wrote the report and the date on which it was dictated
- Objective reports of the patient’s subjective statements, if they are relevant.
- Objective measurements of functional gains in performance.
- Assessment of improvement, extent of progress (or lack thereof) toward each goal;
- Plans for continuing treatment, reference to additional evaluation results, and/or treatment plan revisions should be documented in the clinician’s progress report; and
- Changes to long or short-term goals, discharge, or an updated plan of care that is sent to the physician/NPP for certification of the next interval of treatment.
- Functional documentation is required as part of the progress report at the end of each progress reporting period. It is also required at the time of discharge on the discharge note or summary, as applicable.
Note: “A re-evaluation should not be required before every progress report routinely, but may be appropriate when assessment suggests changes not anticipated in the original plan of care.“
Optional Elements of a Medicare Progress Report
Optional elements may include subjective statements made by the patient related to progress.
Additional optional elements may include information related to communication among other healthcare providers as well as new information related to discharge planning.
Updating and Changing the Original Physical Therapy Plan of Care.
In my experience as a physical therapist, it takes several visits to understand my patient’s condition fully. The first visit is the initial evaluation and treatment. This is like a blind date. The patient and I are putting our best foot forward.
The patient is trying to tell me what he thinks I want to hear and I am trying to dig deep into the root cause of the problem.
After a couple of visits, a level of trust and rapport is established and now the patient often feels more comfortable sharing more personal details.
Since my initial evaluation and plan of care has already been completed and submitted to the referring physician for certification, it isn’t uncommon for me to incorporate new information into the first progress report and as needed update my plan of care to extend the initial certification period. I also often may request additional visits and add new long-term goals.
As I mentioned above, when I add new information and change the certification period I am required by Medicare to acquire an updated signature on the progress report which functions as the updated plan of care.
Summary:
- A physical therapy progress report is not a physical therapy reevaluation.
- A physical therapy progress report is required every 10 treatment visits or sooner according to Medicare Part B guidelines.
- There is no 30-day requirement for PT progress reports under Medicare Part B
- The referring physician or nonphysician provider is not required to sign a standard physical therapy progress report unless that report is adding a new diagnosis or significantly changes the plan of care.
Who is allowed to certify a Medicare physical therapy plan of care? 2022
Which providers are allowed to certify a Medicare physical therapy plan of care? There are several types of healthcare providers that are allowed to certify a Medicare physical therapy plan of care. Medical Doctor Doctor of Osteopathic Medicine Nurse Practitioner Physician's...
How Long Do Physical Therapy Sessions Take? 15, 30, or 60 Min?
My mom asked me "How long do physical therapy sessions take?" not because she was so eager to go, but rather because she wanted to get it over with.https://youtu.be/jwneMxD1jKsThe average physical therapy session at my clinic, Total Therapy Solutions, will last between...
7 TIPS for What to Wear to Physical Therapy
Choosing What to Wear to Physical Therapy Depends on What is Being Treated Physical therapy is a broad profession and encompasses the treatment of many different conditions. A patient receiving treatment for low back pain might dress very differently than a patient receiving...