Bill a Medicare Supplmental Insurance for Physical Therapy Service
Step 1 – Initial insurance verification process.
Before physical therapy services are delivered, you should verify your patient’s health insurance coverage.
To do this, get a copy of the primary and secondary insurance cards. I recommend copying the front and back of both cards since the back of the card often has contact information for the payer.
If you are verifying coverage for Medicare part B you should consider using the MAC portal. In the MAC portal you can verify that your patient does in fact have Medicare part B and not a Medicare advantage plan which is also known as Medicare part C.
In some cases you may be able to verify that the auto-crossover is set up for the supplemental plan within the MAC portal. If you are unsure, you can call your MAC to verify.
Step 2 – Submit your Medicare claim.
If you don’t have time to verify the Medicare supplemental or secondary plan will auto-crossover ahead of time, you may choose to wait until Medicare processes your claim.
In my experience, if the secondary payer is a true supplemental plan (Medigap policy) then it is likely already set up in the Medicare system to automatically cross-over.
How to Know if Medicare will Auto-Forward a Secondary Claim
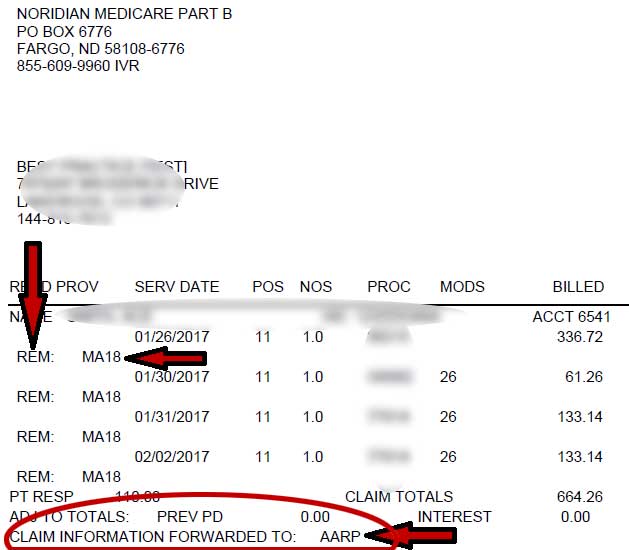
If you didn’t very auto-crossover before submitting the claim, then once Medicare has processed your claim, you will receive an explanation of benefits (EOB) or a electronic remittance advice (ERA). These documents will show you, the provider, how Medicare processed your claim, what was paid, and what the remaining balance might be.
At the bottom of each claim you will see a line of text that reads “Forwarded to …”
See image below:
When does Medicare not auto-forward a claim to the secondary payer?
Medicare does not auto-forward the claim to the secondary payer when the secondary payer is not a supplemental plan.
For example, if the primary policy holder is your patient and your patient is a Medicare beneficiary with an active Medicare part B policy, but your patient has a spouse with health insurance coverage through an employer, that employer sponsored policy is not a supplemental plan.
Since it is a secondary insurance, but not a supplemental plan Medicare will not auto-forward the claim information.
In this case you will have to submit the claim to the seconary insurance with the information from Medicare in the primary position.
Paper Claims – CMS 1500 Claim Form
If you are sending your secondary claim information to a non-supplemental insurance plan you will need the following items:
- Official CMS 1500 claim forms
- Paper copy of your physical therapy practice’s Medicare EOB
- Paper copy of a W9 if you are not contracted with the seconary payer
Electronic Claims – Clearinghouse
If you are sending your secondary claim information via a clearinghouse like Office Ally, Availity, etc you will need to verify that the seconday payer will accept secondary claims via your clearinghouse and determine what additional information or possible formatting you may need for the seconary claim to process.
Summary
In my experience,
- all supplemental plans have auto-crossover already established and there is no need for me to manual submit claims to secondary supplemental plans.
- all non-supplemental secondary plans require paper claims be submitted along with a copy of the original Medicare EOB and CMS 1500 claim form.
- if the secondary is a true Medicare supplemental you are not required to be a participating provider with that specific plan.
- if the secondary plan is not a supplemental then you may be required to be a contracted provider with that third party payer in order to be paid.
Bonus
This cheat sheet is a great resource for addtional information about the Medicare Crossover Process.

