What does ICD 10 Code for Physical Therapy Stand For?
The letters ICD are International Classification of Diseases. In plain language, this is a classification system for establishing an alphanumeric system for coding every diagnosis. While there is no single ICD 10 Code for Physical Therapy, there are several common ICD 10 codes physical therapists will use when treating patients.
Physical Therapist Diagnosis Codes
Physical therapists use a tiny fraction of common ICD-10 diagnosis codes. In my physical therapy clinic, I have a paper list of the most common codes I use on a daily basis. This list is posted near every computer workstation and is updated as needed.
Is there an ICD 10 for Physical Therapy?
There are no ICD 10 codes for physical therapy specifically. The diagnosis codes I will discuss in this article are the most common ones I use in outpatient orthopedic physical therapy.
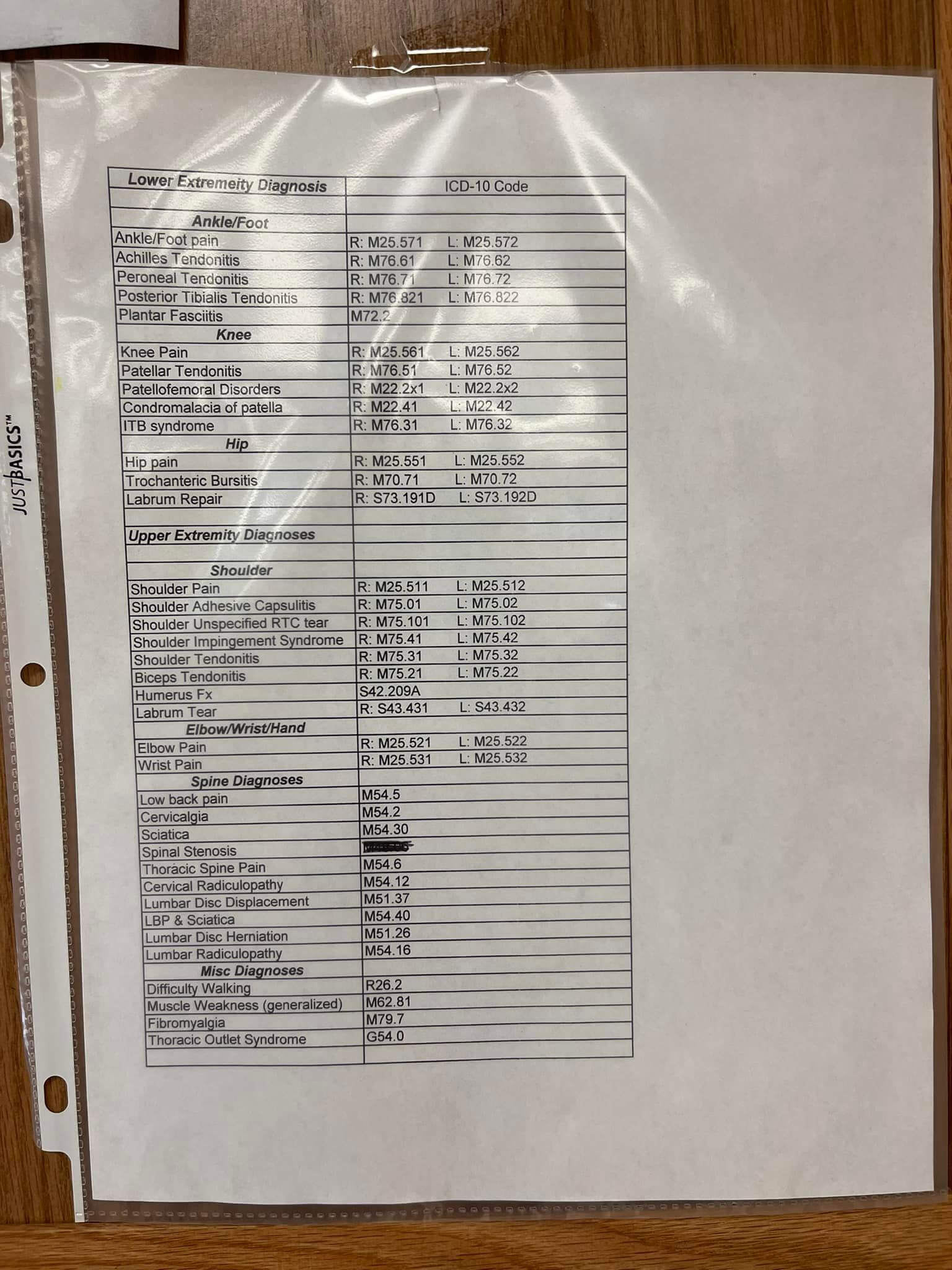
* Note: The above list does not reflect the updated change to ICD 10 code M54.5 which is now M54.50.
ICD 10 code for physical therapy: Outpatient PT
| Condition | Right | Left |
| Shoulder Pain | M25.511 | M25.512 |
| Elbow Pain | M25.521 | M25.522 |
| Wrist Pain | M25.531 | M25.532 |
| Neck Pain | M54.2 | |
| Thoracic Pain | M54.6 | |
| Lumbar Pain | M54.50 | |
| Hip Pain | M25.551 | M25.552 |
| Knee Pain | M25.561 | M25.562 |
| Ankle Pain | M25.571 | M25.572 |
| Difficulty Walking | R26.2 |
* Note: Neck Pain, Thoracic Pain, and Lumbar Pain do not have a left/right designation.
Physical Therapy Treatment Diagnosis vs Medical Diagnosis
The medical diagnosis is often what the referring physician documents on the physical therapy referral. A medical diagnosis might be the surgery performed for the initial encounter diagnosis.
The treatment diagnosis is what the physical therapist will be evaluating and treating during the episode of therapy.
For example, a new patient referred to me for physical therapy might have had a right knee meniscectomy with a medical diagnosis code of meniscectomy ICD 10: S83.241A. Upon my physical therapy evaluation, I determine my physical therapy treatment ICD 10 diagnosis code will be Difficulty Walking: R26.2 or Pain in right knee: M25.561.
Are You Required to Use the ICD Code Listed on the Physical Therapy Referral?
No. Check with your state practice act first, but in most states you are allowed to choose your treatment diagnosis based on your initial evaluation.
Medicare specifically states that “A diagnosis (where allowed by state and local law) and description of the specific problem(s) to be evaluated and/or treated. The diagnosis should be specific and as relevant to the problem to be treated as possible. In many cases, both a medical diagnosis (obtained from a physician/NPP) and an impairment based treatment diagnosis related to treatment are relevant. The treatment diagnosis may or may not be identified by the therapist, depending on their scope of practice. Where a diagnosis is not allowed, use a condition description similar to the appropriate ICD code.”
“This section goes on to say “For example the medical diagnosis made by the physician is CVA; however, the treatment diagnosis or condition description for PT may be abnormality of gait, for OT, it may be hemiparesis, and for SLP, it may be dysphagia. For PT and OT, be sure to include body part evaluated. Include all conditions and complexities that may impact the treatment. A description might include, for example, the premorbid function, date of onset, and current function;” Reference Link
What if the physician referral for physical therapy does not have an ICD 10 Code?
As mentioned above, first determine if you are allowed to establish a treatment diagnosis and then confirm that the payer will allow you to choose a treatment diagnosis.
Here in Ohio, the bureau of workers compensation requires physical therapists only use the diagnosis codes approved on the C-9 form. Services delivered for any other diagnosis will be denied for payment.
Medicare part B does not require a referral from a physician, so as long as your state practice act allows it, you may choose the treatment diagnosis based on your clinical examination and evaluation.
Does ICD 10 Code Choice Affect Reimbursement?
No! Currently, the choice of ICD 10 code does not affect reimbursement rates for standard physical therapy, occupational therapy, and speech-language pathology procedure codes.
Should a PT Include Multiple ICD 10 Codes on a Claim?
Physical therapists should include all applicable ICD 10 codes for conditions that were evaluated at the start of care.
It is possible that a second evaluation is performed after the episode of care has started. For example, if a second condition initiates while performing therapy for the first condition, a second evaluation may be billed and additional treatment diagnosis codes would be added to the claim.
Summary:
- Choose the most specific diagnosis code based on your clinical evaluation.
- Don’t try to get fancy. Simply codes reimburse the same rate as a more complex ICD 10 Code for Physical Therapy.
- Create your own cheatsheet for physical therapy ICD 10 codes to make it easy to find the best code.
How To Create A Telehealth Claim For Physical Therapy, OT or SLP United Healthcare
Telehealth is a hot topic for physical therapy, occupational therapy, and speech therapy due to the COVID19 virus. As insurance payers continue to increase access to telehealth services and telerehabilitation, it is important for clinicians to know how exactly to submit claims for telehealth reimbursement.
How to submit a telehealth claim for Anthem BCBS for PT OT SLP in 2020
Learning how to create a submit a telehealth claim for physical therapy, occupational therapy, and speech therapy can be an important skillset right now during the global pandemic and social distancing. In this video I show you what Anthem BCBS of Georgia is requiring you do to create a CMS 1500 claim for telehealth services.

Do you need to become a physical therapist to deliver the value of a physical therapist?
Do you need to become a physical therapist to deliver the value of a physical therapist?

Comparing Reimbursement for 3 Different Medicare Advantage Plans – $FREE
How can you decide to join a payer network when you have no idea what the contract will pay or what your obligations will be?
In this 18:32 video I review three different Medicare Advantage plan reimbursements from a 2019 fee schedule along with sharing some tips and bonus information that may help you know what to look for when deciding to join a payer network.

