Medicare’s Definition of a Treatment Day
Medicare defines a treatment day as a single calendar day. A physical therapist might deliver multiple treatment sessions in a single treatment day.
For the purposes of physical therapy progress reports, Medicare Part B requires a progress report be completed no less than once every 10 treatment days.
Medicare Definition of a Treatment Day Outpatient Physical Therapy
Treatment Day
Why is this important?
According to Medicare Benefit Policy Manual page 191 “The minimum progress report period shall be at least once every 10 treatment days.”
How does this impact a typical physical therapy plan of care?
In my PT clinic, there may be times when a patient receives two therapy visits in a single treatment day.
Today for example I had a patient walk in to schedule an initial evaluation. He was planning on scheduling the evaluation for a later time that same day or another day.
Since I was available, I initiated the initial evaluation and interview process right then. I collected his case history and symptoms while I was copying his insurance cards and collecting his information. Before he left 10 minutes later, I not only scheduled him to return the same day at 3:30 PM, but I also observed several functional activities and started entering that information into my initial evaluation.
At that time I had everything I needed for an initial evaluation report and plan of care. According to the Medicare Benefit Policy Manual, a plan of care requires a diagnosis, long-term goals, type, duration, and frequency.
I also had most of what I needed to formally complete my initial evaluation report which included the assessment of his walking, bending, stooping, and reaching. I was able to watch him open the door, and transfer to/from his car. I was able to watch his fine motor dexterity when he signed my initial paperwork and while he was getting his insurance cards and driver’s license out of his wallet.
Therapists often take for granted our evaluative skills and assessment. If I later determined that I needed range of motion or some other more technical measure I could do that upon his return.
After the 10-minute interview, evaluation, and assessment I created his plan of care, sent it to his referring physician, and scheduled him for his second physical therapy treatment on the same treatment day with my physical therapist assistant.
CPT Code Therex 97110
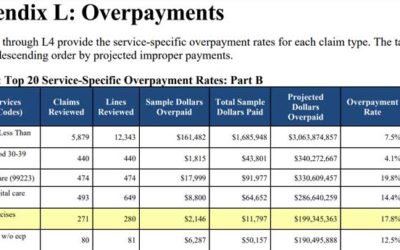
CPT Code Therex 97110 CPT Code Therex 97110 (Therapeutic Exercise) was the 4th highest ranked procedure code listed on the 2021 CMS CERT Overpayment Top 20 List.What is the...
Medicare Provider Enrollment Rejection
Nothing is more frustrating than when you Medicare provider enrollment rejection notice arrives in your email inbox. What happens if your physical therapy Medicare provider...
Does Medicare Cover Massage Therapy
Massage therapy is only a covered service for Medicare when it is provided as part of a comprehensive treatment. When providing massage only it is not a covered service and therefore providers are allowed to provide it to Medicare beneficiaries for cash pay (self pay) physical therapy.