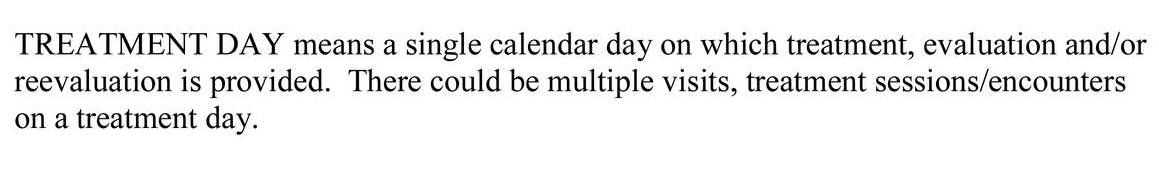
Medicare’s Definition of a Treatment Day
Medicare defines a treatment day as a single calendar day. A physical therapist might deliver multiple treatment sessions in a single treatment day.
For the purposes of physical therapy progress reports, Medicare Part B requires a progress report be completed no less than once every 10 treatment days.
Medicare Definition of a Treatment Day Outpatient Physical Therapy
Treatment Day
Why is this important?
According to Medicare Benefit Policy Manual page 191 “The minimum progress report period shall be at least once every 10 treatment days.”
How does this impact a typical physical therapy plan of care?
In my PT clinic, there may be times when a patient receives two therapy visits in a single treatment day.
Today for example I had a patient walk in to schedule an initial evaluation. He was planning on scheduling the evaluation for a later time that same day or another day.
Since I was available, I initiated the initial evaluation and interview process right then. I collected his case history and symptoms while I was copying his insurance cards and collecting his information. Before he left 10 minutes later, I not only scheduled him to return the same day at 3:30 PM, but I also observed several functional activities and started entering that information into my initial evaluation.
At that time I had everything I needed for an initial evaluation report and plan of care. According to the Medicare Benefit Policy Manual, a plan of care requires a diagnosis, long-term goals, type, duration, and frequency.
I also had most of what I needed to formally complete my initial evaluation report which included the assessment of his walking, bending, stooping, and reaching. I was able to watch him open the door, and transfer to/from his car. I was able to watch his fine motor dexterity when he signed my initial paperwork and while he was getting his insurance cards and driver’s license out of his wallet.
Therapists often take for granted our evaluative skills and assessment. If I later determined that I needed range of motion or some other more technical measure I could do that upon his return.
After the 10-minute interview, evaluation, and assessment I created his plan of care, sent it to his referring physician, and scheduled him for his second physical therapy treatment on the same treatment day with my physical therapist assistant.
Medicare Guidelines for Billing Therapeutic Exercise 97110 PT, OT in 2020
“Many therapeutic exercises may require the unique skills of a therapist to evaluate the patient’s abilities, design the program, and instruct the patient or caregiver in safe completion of the special technique. However, after the teaching has been successfully completed, repetition of the exercise, and monitoring for the completion of the task, in the absence of additional skilled care, is non-covered. For example, as part of the initial therapy program following total knee arthroplasty (TKA), a patient may start a session on the exercise bike to begin gentle range of motion activity. Initially the patient requires skilled progression in the program from pedal-rocks, building to full revolutions, perhaps assessing and varying the
seat height and resistance along the way. Once the patient is able to safely exercise on the bike, no longer requiring frequent assessment and progression, even if set up is required, the bike now becomes an “independent” program and is no longer covered by Medicare.”
How To Create A Telehealth Claim For Physical Therapy, OT or SLP United Healthcare
Telehealth is a hot topic for physical therapy, occupational therapy, and speech therapy due to the COVID19 virus. As insurance payers continue to increase access to telehealth services and telerehabilitation, it is important for clinicians to know how exactly to submit claims for telehealth reimbursement.
How to submit a telehealth claim for Anthem BCBS for PT OT SLP in 2020
Learning how to create a submit a telehealth claim for physical therapy, occupational therapy, and speech therapy can be an important skillset right now during the global pandemic and social distancing. In this video I show you what Anthem BCBS of Georgia is requiring you do to create a CMS 1500 claim for telehealth services.