A letter of medical necessity is simply a document supporting the need for a prescribed assistive device that may be used by the patient to improve or treat a medical condition.
If a physical therapist determines a patient may require a walker to assist in ambulation, maintain or improve independence, and reduce the risk of falling, then a letter of medical necessity would document why the patient needs this device, how long the patient will use the device, and how the device will support patient independence.
What should a letter of medical necessity contain?
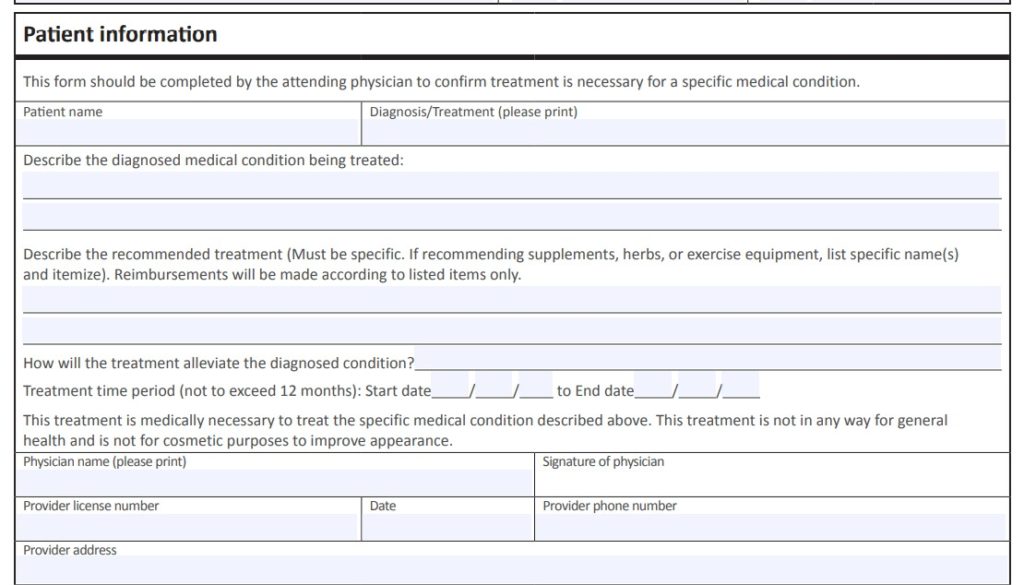
- Patient Name
- Patient Diagnosis
- Date
- Provider Name
- Patient Demographic Information: Date of birth, address, insurance information
- Specific equipment or treatment being recommended
- The recommended treatment must be described by your licensed healthcare provider.
- For example, a recommended exercise program through a gym membership for the next six months to alleviate the patient’s hypertension.
- Duration of the treatment or length of use for the equipment
- For example, is the equipment going to be a rental or purchase? How many weeks, months?
- A provider may recommend a specific duration of treatment recommended
- Signature of the licensed practitioner writing the letter of medical necessity.
- Supporting documentation from the medical record.
- For example, imaging reports, a doctor’s prescription, case manager, or social worker report.
What is an example of medical necessity?
Different insurance providers may have their unique specifications of what medical necessity actually is and what is actually covered within the insurance policy benefit.
Medicare Part B defines medical necessity as “Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice.”
In terms of physical, occupational, and speech therapy services, Medicare also defines medically necessary service as those services of such complexity that they “require the skills of a therapist.”
For more information research your specific third-party payer’s website for coverage and reimbursement guidelines.
How do you end a letter of medical necessity?
End with a clear and objective recommendation. If your patient requires a wheelchair then that is what should be requested.
Everything prior to the final request is supporting documentation.
Be sure to be clear and concise. Precision can go a long way in helping justify the request.
How long is a letter of medical necessity good for?
Different third-party payer guidelines will specify how long a letter of medical necessity may be valid.
Generally, plans range between 30-days and 12-months.
Additional and Related Article Links:
How to INCREASE the Average Physical Therapist Salary
5 Best Books For Starting A New Physical Therapy Practice in 2021

Anthony Maritato, PT
Physical Therapist / Private Practice Owner
As a serial entrepreneur since the age of 7, Anthony (Tony) Maritato didn’t start his first physical therapy clinic until he was 26.
After recently graduating from Pennsylvania State University with a bachelor’s degree in Kinesiology, Tony fell in love with the profession of physical therapy. Not wanting to wait until getting his degree in Physical Therapy, Tony quickly opened a personal training studio which transitioned to a full-time physical therapy clinic once he recruited his now-wife, Kathy Long Maritato, PT.
Since then Kathy and Tony have grown Total Therapy Solutions LLC into a successful private practice with two locations in Ohio.
Tony spends his free time teaching other therapists how to contract with and bill Medicare for outpatient therapy services.