CashPT for Medicare Beneficiaries Who Want Something Better
Mandatory Claim Submission Law
40.33 – Mandatory Claims Submission (Rev. 222, Issued: 05-13-16, Effective: 08-15-16, Implementation; 08-15-16) Section 1848(g)(4) of the Act, “Physician/Practitioner Submission of Claims,” regarding mandatory claims submission, does not apply once a physician or practitioner signs and submits an affidavit to the Medicare contractor opting out of the Medicare program, for the duration of the physician’s or practitioner’s opt-out period, unless the physician or practitioner knowingly and willfully violates a term of the affidavit.
Other Non-Covered Medicare Services for CashPTs
- Anything related to recreation and sports.
- Services that have been deemed as not medically necessary by the patient’s physician.
- Services rendered in a location other than the patient’s home or your clinic.
- Services delivered by asynchronous electronic communication such as email or text messaging.
- Asynchronous video programming.
- Some versions of home exercise programs.
- Services delivered by someone other than a licensed therapist or assistant working under the direct supervision of a therapist.
Build Your Provider Network
If I were still in the cashPT only business model I would network with other Medicare contracted providers to build my provider network.
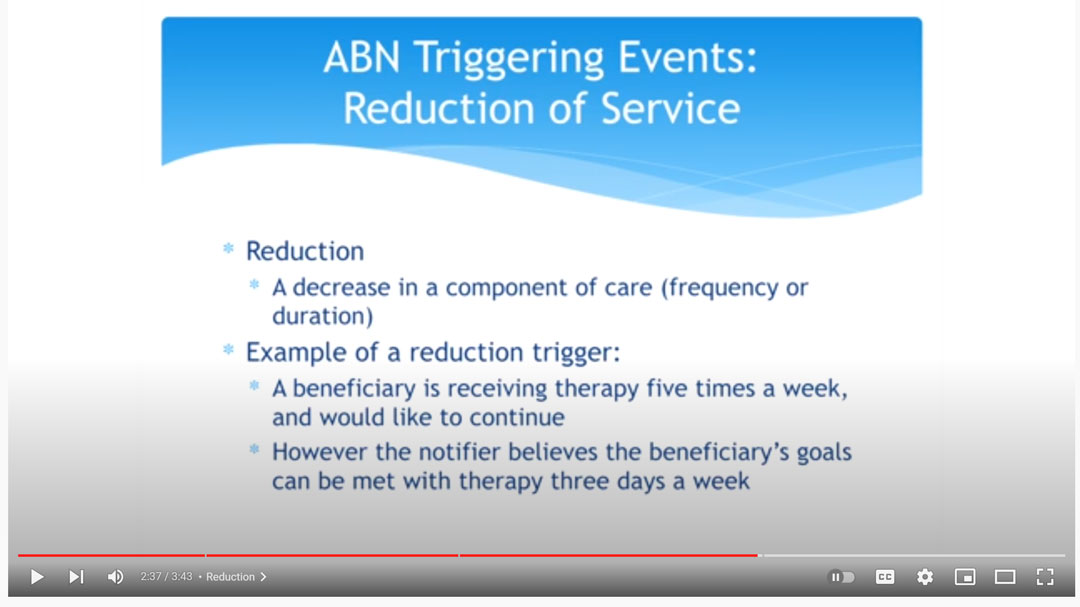
In this video, NGSMedicare MAC explains how when a patient wants 5 days a week of physical therapy services, but only 2 days a week is medically necessary, the patient may choose to self pay for the additional three days a week.
In this case, an ABN would be issued by the contracted provider if the contracted provider is supplying the additional 3 days a week of treatment.
If the extra treatments are provided by an unaffiliated physical therapist no ABN is issued.
Can a CashPT use an ABN?
No. Only Medicare contracted participating and non-participating providers may use a CMS Advance Beneficiary Notice (ABN).
Medicare Advantage
Does the ABN apply to Medicare Advantage plans?
No. The ABN is not applicable to Medicare Advantage insurance plans. Keep in mind that the Mandatory claim submission law does not apply to Medicare Advantage plans. Physical therapists that are not affiliated with Medicare Part B in any way are allowed to treat patients with Medicare Advantage insurance.
Can a Contracted Medicare Provider Offer CashPT?
Yes! The best of both worlds is to become a contracted Medicare provider who offers both Medicare covered and non-covered services.
For example, Medicare does not cover dry needling CPT Code 20560 and CPT Code 20561 when delivered by a licensed physical therapist. If you are a contracted Medicare provider your initial physical therapy evaluation would be a covered service, then if you determined that dry needling would benefit your patient and you are capable of delivering the dry needling intervention you would be allowed to charge a self pay rate for the dry needling intervention.
Medicare Covered Initial Evaluation and Dry Needling CashPT
In this case, Medicare would reimburse the Medicare allowed amount for the physical therapy evaluation CPT Code 97161 – $98 and you would charge the patient your standard CashPT rate for CPT Code 20560 – $60.
The total revenue for a 30-minute session would be $158.
Both of these services may be provided in the same day. You may choose to supply an optional ABN as a courtesy to your patient, but it is not required.
Summary:
- The federal mandatory claim submission law requires all healthcare providers to submit claims for service to Medicare when providing Medicare-covered services.
- If you are a cashpt with no affiliation to Medicare Part B and you want to help Medicare beneficiaries an easy way to accomplish this is to work with a contracted Medicare provider.
- If you become a contracted Medicare provider you would be allowed to provide both covered and non-covered services.
Read more:
7 TIPS for What to Wear to Physical Therapy
Choosing What to Wear to Physical Therapy Depends on What is Being Treated Physical therapy is a broad profession and encompasses the treatment of many different conditions. A patient receiving treatment for low back pain might dress very differently than a patient...
7 BEST Physical Therapy SEO Tips for Private Practice
You Found This Article Because of Physical Therapy SEO! We are going to reverse engineer the physical therapy SEO strategy that brought you to this article. What is SEO? SEO stands for search engine optimization. Before you found this webpage, you had a problem and you...
Physical Therapy ReEvaluation CPT Code 97164
What is a Physical Therapy Reevaluation CPT Code 97164? According to Medicare A53309 CPT Code 97164: "Re-evaluations are separately reimbursable when the medical record supports that the patient's clinical status or condition required the additional evaluative service....
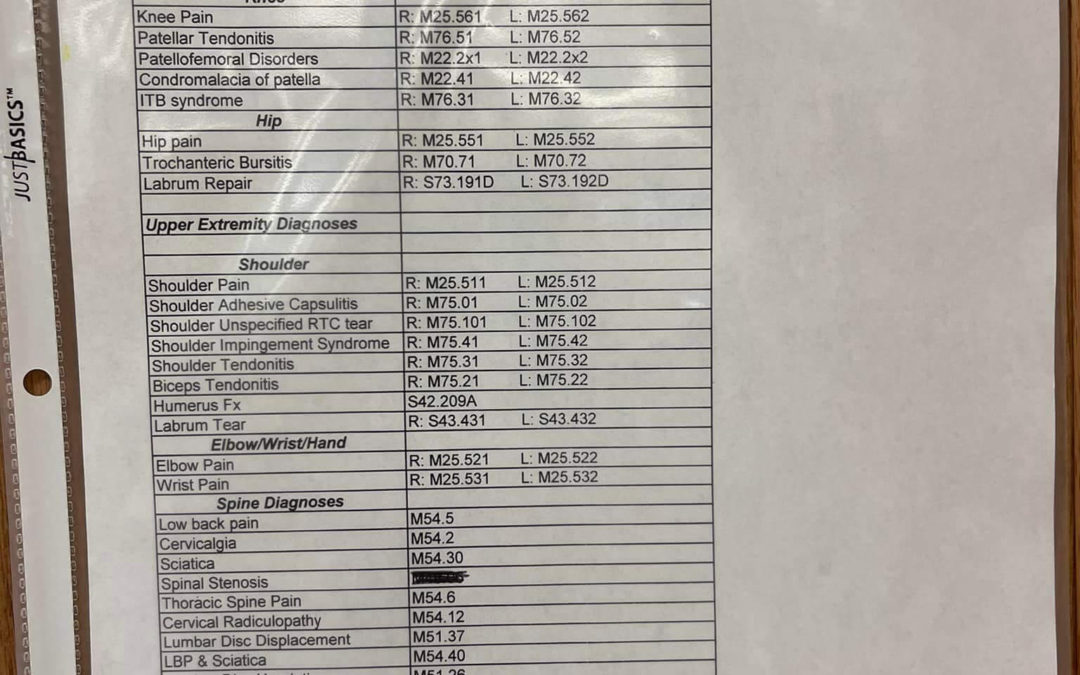
Common ICD 10 Code for Physical Therapy: Outpatient Orthopedic
What does ICD 10 Code for Physical Therapy Stand For? The letters ICD are International Classification of Diseases. In plain language, this is a classification system for establishing an alphanumeric system for coding every diagnosis. While there is no single ICD 10 Code...

How much does AFLAC Pay for Physical Therapy?
How Much Does AFLAC Pay for Physical Therapy? According to AFLAC's therapy Accident Advantage plan, "THERAPY BENEFIT: Aflac will pay $35 per therapy treatment when a Covered Person receives treatment for Accidental Injuries sustained in a covered accident and later a...