Reference links: Billing and Coding: Lymphedema Decongestive Treatment
- Article ID: A52959, A53287
CPT Code 29581 – Definition
CPT Code 29581 – Application of multi-layer compression system; leg (below knee), including ankle and foot [1]
Examples of graduated, high-compression bandage systems?
- Profore®
- Dyna-Flex®
- Surepress®
- Setopress®
Am I allowed to bill 97140 on the same visit as CPT Code 29581?
“97140 – Should not be reported for any type of manual therapy provided during the same patient encounter in the same anatomic region where [CPT Code 29581] a multi-layer compression system is applied.”
Am I allowed to bill 97597 on the same visit as CPT Code 29581?
“97597 – Should not be reported with casting/splinting/strapping (CPT Code 29580 or CPT Code 29581) for the same anatomic area.”
What is Manual Lymphatic Drainage (MLD)
Manual Lymphatic Drainage (MLD) which stimulates the movement of fluids in the tissues using gentle massage
What is Comprehensive Decongestive Therapy (CDT)
Comprehensive Decongestive Therapy (CDT) which is a combination of MLD, bandaging, skin care and exercises
Coverage Requirements
Medicare will reimburse for necessary components of decongestive treatment when the medical record supports
- A diagnosis of lymphedema (not tissue edema due to other etiologies e.g., chronic venous insufficiency, congestive heart failure, acute infection).
- Recent changes in the patient’s condition
- Prior unsuccessful therapies (e.g., elevation, bandaging, diuresis) reported to justify the need for skilled services.
- Services were provided by a qualified clinician (i.e., physician, non-physician practitioner (NPP), qualified therapist, or appropriately supervised therapist assistant).
- Services must be under accepted standards of medical practice and considered to be specific and effective treatment for the patient’s condition.
Limitations
The goal of therapy is not to achieve maximum volume reduction but to ultimately transfer the responsibility for the care from the provider to the patient and/or caregiver, generally within a 1-3 week time period.
There is only temporary benefit from the treatment unless the patient and/or caregiver are able to complete treatments at home on an ongoing basis. The end of treatment is not when the edema resolves or stabilizes but when the patient and/or caregiver are able to continue the treatments at home.
* I would personally add that the end of treatment may also occur when it has been determined that the patient or caregiver is unable or unwilling to continue the treatments at home.
Skilled Level of Care
The key issue is whether the skills of a therapist are needed, or whether the services can be carried out by the patient and/or caregiver after sufficient training.
The medical record must clearly indicate the patient’s condition before, during, and after the therapy episode to support that the patient significantly benefitted from ongoing therapy services and that the progress was sustainable and of practical value when measured against the patient’s condition at the start of treatment.
Documentation should indicate clear objective evidence of improvement generally within the first week or 10 days of therapy (e.g., changes in weight, extremity circumference).
Objective Criteria Examples:
- Before treatment on 3/6/2022 the limb weight was 13.4-lbs
- After treatment on 3/6/2022 the limb weight was 12.1-lbs
- Before treatment on 3/8/2022 the limb weight was 12.5-lbs
- After treatment on 3/8/2022the limb weight was 11.7-lbs
In the example above both improvement and retention of improvement was evidenced by the carried over improvement. Adding to the measurements would be a narrative statement indicating the patient’s compliance between sessions.
Maintenance Level of Care
When it is reasonable to assume that ongoing services could reasonably be carried out by the patient and/or appropriately trained caregiver(s), then the services are considered to be at a maintenance level of care and no longer require the skills of a qualified clinician.
* Don’t confuse this maintenance therapy with covered maintenance therapy. In this situtation the policy is referencing non-covered maintenance.
It is the patient’s responsibility to acquire caregiver assistance for carrying out the of the home maintenance program when necessary.
Generally, it is anticipated that an efficient home maintenance program will be effective for a lifetime. However, in the rare instance, when additional treatment for the same condition is necessary, then the documentation must support reasonableness and medical necessity for the additional services.
For additional information, see the Noridian article titled “Medical Necessity of Therapy Services“.
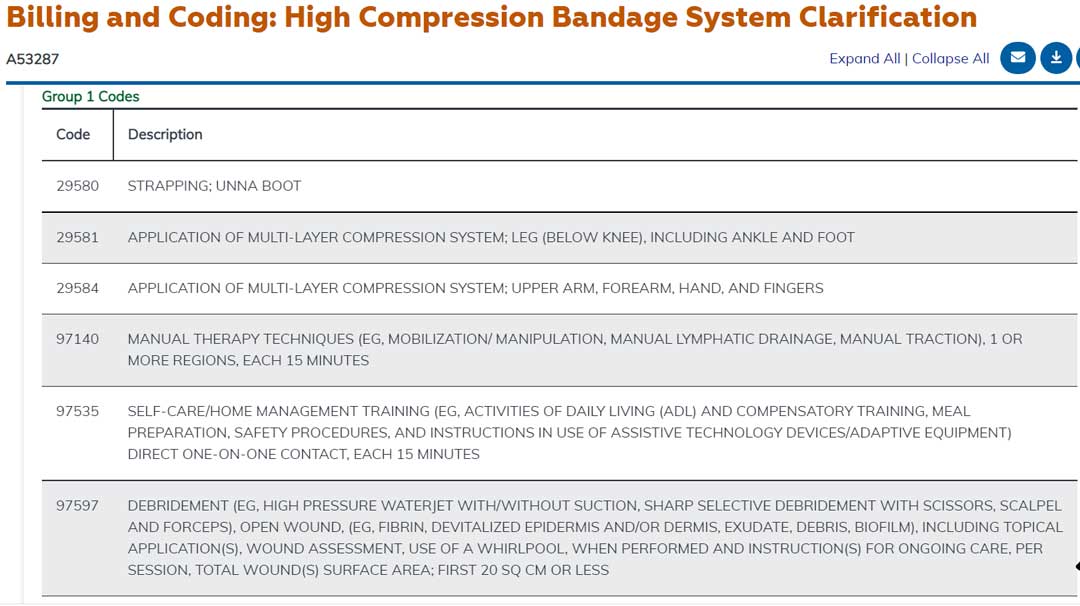
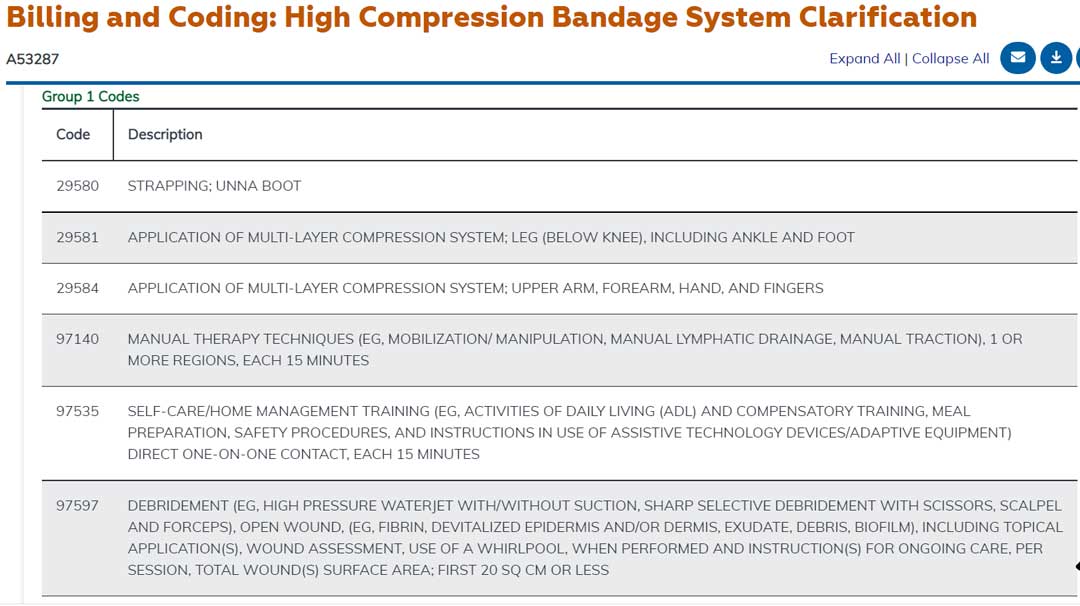
Coding Considerations
- Medically necessary hands-on MLD is a covered Medicare service and is coded using CPT® 97140 for manual therapy.
- There is no Medicare coverage for lymphedema compression bandage application as this is considered to be an unskilled service. This non-coverage extends to the application of high compression, multi-layered, sustained bandage systems (e.g., Profore®, Dynaflex®, Supress®, coded with CPT® 29581 or 29584.
- Minutes spent applying compression bandaging without patient/caregiver education should not be billed as skilled therapy services.
- However, Medicare will cover a brief period (e.g. three or fewer sessions if no new specific issues are identified), of patient/caregiver instruction in compression bandaging home management. Medical necessity for this education must be clearly documented and meet the code descriptor requirements for CPT® 97535.
- Note that high compression bandage application used for treatment of wounds may be appropriately coded with CPT® 29581 or 29584. However, these codes should not be billed for unskilled lymphedema compression bandage application. For additional information, see the Noridian article titled “High Compression Bandage System Clarification.”
Additional Resources:
National Correct Coding Initiative (NCCI) Policy Manual Hospital APC Version 19.2, Chapter IV, Part F, Sections 3 and 15