How Much Does AFLAC Pay for Physical Therapy?
According to AFLAC’s therapy Accident Advantage plan, “THERAPY BENEFIT: Aflac will pay $35 per therapy treatment when a Covered Person receives treatment for Accidental Injuries sustained in a covered accident and later a Physician advises the Covered Person to seek treatment from a licensed Occupational, Physical, or Speech Therapist. Occupational, physical, or speech therapy must be for Accidental Injuries sustained in a covered accident and must start within 30 days of the covered accident or discharge from the Hospital. Aflac will pay for one treatment per day for up to a maximum of ten treatments per covered accident, per Covered Person. The treatment must take place within six months after the accident. The Therapy Benefit is not payable for the same days that the Accident Follow-Up Treatment Benefit is paid. “
What kind of Therapy is Covered?
The really great part about this coverage is that it includes occupational therapy, speech therapy, and physical therapy.
Does the 10-visit limit include all 3 therapy disciplines?
Yes, the 10-visit limit includes all three disciplines. That means, for example, that you could receive the $35 reimbursement for each of 4 PT treatments, 4 OT treatments, and 2 SLP treatments.
What are the requirements for coverage?
- AFLAC requires the patient have a physician referral. Even if your state offers direct access, a physician referral is required for AFLAC coverage of therapy services.
- The therapy services must start within 30-days of the accident. Also, the 10-covered therapy visits must be completed within 6-months of the accident. The best advice is to complete an initial evaluation within 30-days of the accident, then complete the first 10-visits within 6 months or sooner.
- AFLAC will pay for up to 6 accident follow-up treatments. These are paid at a rate of $35 per session and can not be provided on the same day as a therapy session. After care follow-up treatment includes accupunture.
Does AFLAC Pay for Telehealth Physical Therapy?
Yes! As long as your state practice act allows the delivery of telehealth physical therapy, this would qualify for the therapy benefit reimbursement.
All the same rules apply as above for in-person therapy.
Does AFLAC Pay for Back Braces and Other Appliances?
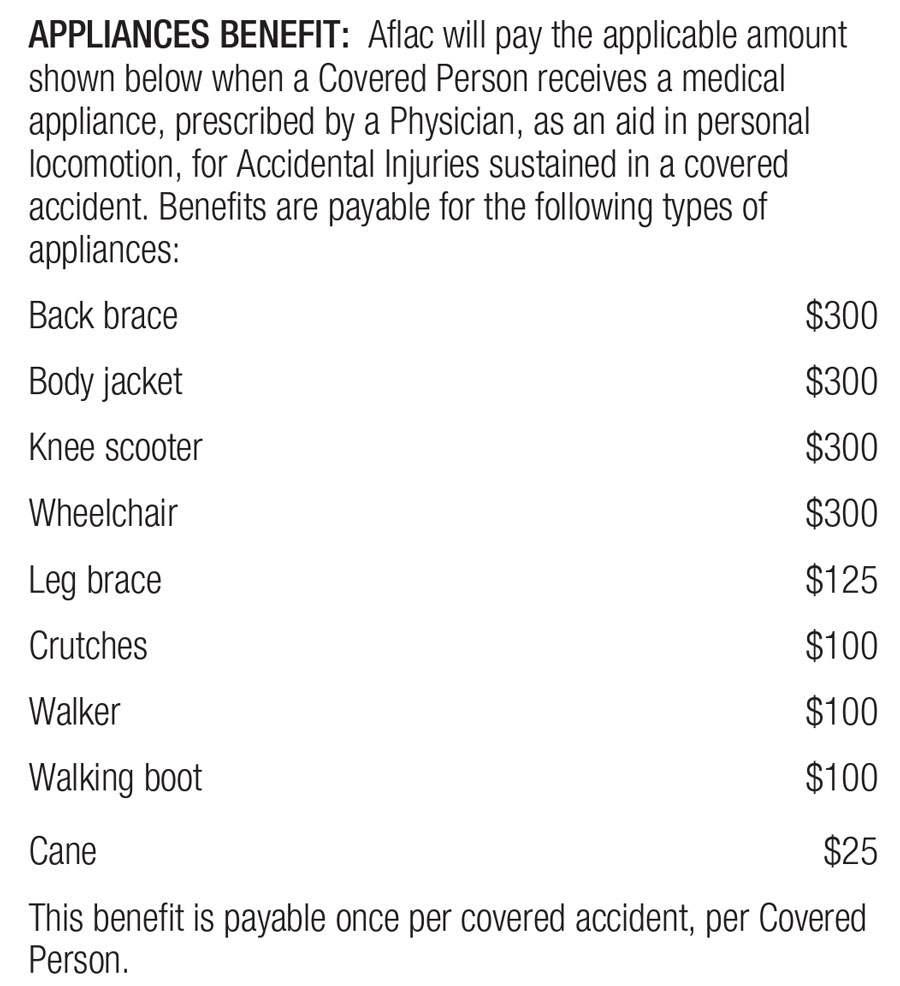
Yes! AFLAC covers several medical devices. “APPLIANCES BENEFIT: Aflac will pay the applicable amount shown below when a Covered Person receives a medical appliance, prescribed by a Physician, as an aid in personal locomotion, for Accidental Injuries sustained in a covered accident. Benefits are payable for the following types of appliances:”
| Back Brace | $300 |
| Body Jacket | $300 |
| Knee Scooter | $300 |
| Wheelchair | $300 |
| Leg Brace | $125 |
| Crutches | $100 |
| Walker | $100 |
| Walking Boot | $100 |
| Cane | $25 |
Does AFLAC Pay for Home Modifications?
Again, yes! “Aflac will pay $3,000 for a home modification aid when a Covered Person suffers a Catastrophic Loss in a covered accident. This benefit is payable once per covered accident, per Covered Person.”
Summary:
AFLAC offers some pretty amazing insurance coverage for commonly used services. Unfortunately, too many people don’t realize they have coverage for these services. If you have questions, review your AFLAC policy guide or call your AFLAC representative.
- AFLAC insurance pays for physical therapy, occupational therapy, and speech-language pathology.
- AFLAC also pays for several common medical devices you may need.
- Finally, AFLAC may pay for a portion of your required home modification following an accident or injury.
Medicare Provider Enrollment Rejection
Nothing is more frustrating than when you Medicare provider enrollment rejection notice arrives in your email inbox. What happens if your physical therapy Medicare provider enrollment application is denied? If you are a physical therapist applying to become a...
Does Medicare Cover Massage Therapy
Massage therapy is only a covered service for Medicare when it is provided as part of a comprehensive treatment. When providing massage only it is not a covered service and therefore providers are allowed to provide it to Medicare beneficiaries for cash pay (self pay) physical therapy.
Best Physical Therapy YouTube Channels in 2022
This article is a YouTube channel roundup of 2022's BEST Physical Therapy YouTube Channels. Selection Criteria... My Personal Opinion! This is a growing list. I will be adding channels as I find them. Check back regularly to see new listings.Physical Therapy YouTube...
CPT Code 97010 Does Insurance Pay for Ice Packs
Does Insurance Pay for CPT Code 97010 Technically, yes, UnitedHealthcare does pay for CPT code 97010, (Application of a modality to one or more areas; hot or cold packs). I say "technically" because it is paid as a bundled payment. Ice packs, moist heat, and other...
Good Faith Estimate and No Surprise Act for Physical Therapy in 2022
In this video interview with Nancy Beckley from https://nancybeckley.com/ d we discuss: Good Faith Estimate No Surprise Act Physical Therapy Billing Occupational Therapy Billing Medicare, Medicaid, Self Pay Services, and more. Highlights and Resources: 45 CFR...