How much does Medicare pay for physical therapy
This article will specifically reference the Medicare Part B Physician Fee Schedule look-up tool to determine how much does Medicare pay for physical therapy.
Medicare Part B payment rates for a physical therapy initial evaluation CPT code 97161?
Medicare Part B has reduced physical therapy rates from $98.01 in 2021 to $95.13 in 2023. This change is specifically for outpatient physical therapy reimbursement in the state of Ohio.
To determine Medicare Part B reimbursement allowed amounts for the calendar year and geographic location you will need to either go to your local MAC website and search their physician fee schedule, or you can find the same information on the CMS website under Physician Fee Schedule Look-Up Tool.
Below is a table showing Medicare Part B allowed amounts for participating providers in Ohio.
Medicare allowed amount by CPT Code: 97110, 97530, and 97140?
Below is a table containing the CMS Physician Fee Schedule allowed amounts for participating physical therapy providers. This table compares reimbursement rates between 2023 and 2021 for Ohio’s CGS Medicare.
Reimbursement will vary by state so it is important that you choose your specific MAC or location.
You can see that the Medicare Part B participating provider allowed amounts are as follows:
| CPT Code | 2023 Payment | 2021 Payment |
| 97110 | $27.89 | $29.21 |
| 97112 | $31.96 | $33.82 |
| 97140 | $25.72 | $26.92 |
| 97161 | $95.13 | $98.01 |
| 97530 | $34.80 | $37.46 |
What is the difference between Facility and Non-Facility Price?
Physical therapists, occupational therapists, and speech-language pathologists in private practice use the Non-facility price to estimate the allowed amount.
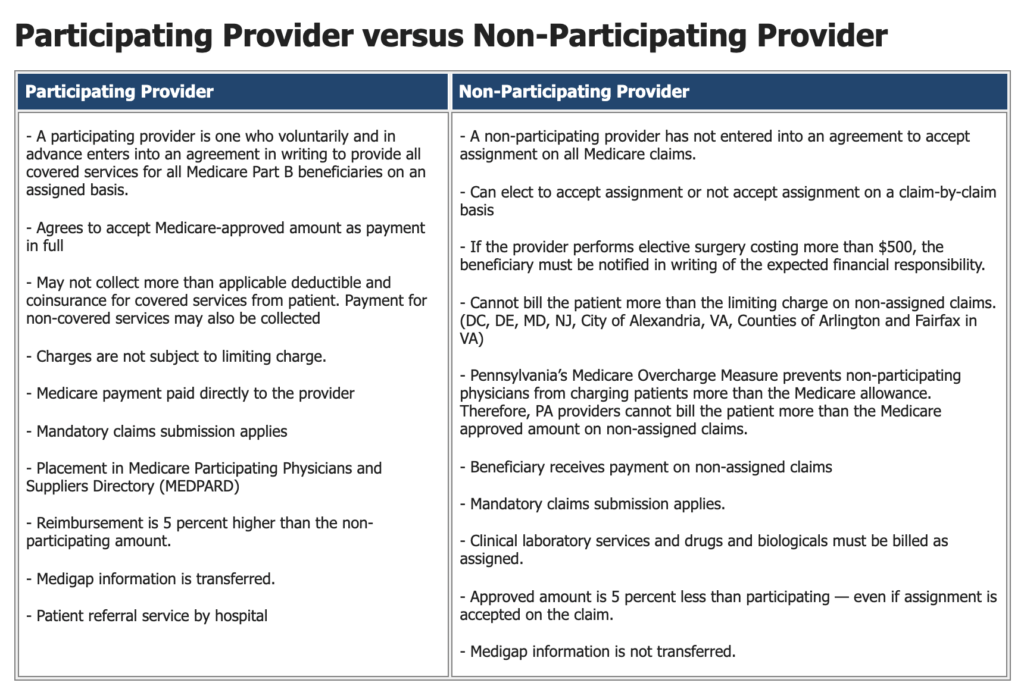
What is the difference between PAR and NonPAR allowed amounts?
The NonPAR allowed amount is 95% of the PAR allowed amount.
* Source: Novitas-Solutions
Is it better for a physical therapist to be PAR or NonPAR?
In my opinion, it is NOT better for a physical therapist, occupational therapist, or speech-language pathologist to be Non-PAR (non-participating).
In the following video, I will share the reasons why Non-PAR is not better, but to summarize it here I have created a list:
- Both participating and non-participating providers are required to comply with all of the same Medicare regulations.
- Both participating and non-participating providers are required to submit claims on behalf of the beneficiary for covered services, but Non-PAR claims are not automatically forwarded to the patient’s supplemental insurance.
- Yes, it is true the Non-PAR provider may choose not to accept assignment and charge the Medicare beneficiary up to 115% of the Non-PAR fee schedule, but the Non-PAR fee schedule is lower and the provider must collect from the patient either at the time of service or after. This results in increased administrative costs.
- If a single Medicare beneficiary chooses not to pay a Non-PAR provider then the cost of collections and other measures may eliminate the potential small increase in reimbursement.
Does Medicare Part B have a CAP on Physical Therapy Services?
No, Medicare Part B no longer has a cap. Now it is referred to as a financial threshold. Click here for information directly from CMS.
In 2023 the Medicare financial threshold for occupational therapy services is $2,230.
The Medicare financial threshold for physical therapy and speech-language pathology combined is $2,230.
What happens if physical therapy services exceed the financial threshold?
If therapy services continue to be medically necessary based on established CMS guidelines, local MAC published guidelines, and the clinical judgement of the provider, then the KX modifier may be added to the CPT code claim line item and payment will be issued from Medicare.
If therapy services are deemed no longer medically necessary AND the patient wants to continue to receive therapy services while paying out of pocket then the provider may choose to issue a mandatory advanced beneficiary notice (ABN) before continuing care.
What if a Medicare beneficiary does not have a secondary insurance plan?
If the Medicare beneficiary does not have a secondary insurance policy that Medicare part B will cover 80% of the allowed amount and the patient will be responsible to pay the remaining 20%.
The best practice for the physical therapist in this situation is to estimate the 20% coinsurance and collect that amount from the patient at the time of service.
After Medicare has processed the claims the physical therapist may review the Medicare determined 20% patient responsibility and either refund the patient if more than expected was collected or invoice the patient if a remaining balance exists.
Does a Medicare secondary insurance plan pay for out-of-network physical therapy?
A traditional Medicare supplemental plan in the secondary position will pay therapists contracted with Medicare just the same as if the therapist was contracted with the supplemental payer.
But non-supplemental secondary insurance plans are not required to pay non-contracted therapists. Each plan is different so you will need to verify coverage and determine any patient responsibility before delivering treatment.
How can I learn more?
The first Tuesday of each month I start a new LIVE cohort of students in my Zero to Paid Medicare Billing Course. For more information on the course visit this website’s homepage.
Additional and Related Article Links:
- How to apply for a Type 2 NPI
- How to INCREASE the Average Physical Therapist Salary
- 5 Best Books For Starting A New Physical Therapy Practice in 2021

Anthony Maritato, PT
Physical Therapist / Private Practice Owner
As a serial entrepreneur since the age of 7, Anthony (Tony) Maritato didn’t start his first physical therapy clinic until he was 26.
After recently graduating from Pennsylvania State University with a bachelor’s degree in Kinesiology, Tony fell in love with the profession of physical therapy. Not wanting to wait until getting his degree in Physical Therapy, Tony quickly opened a personal training studio which transitioned to a full-time physical therapy clinic once he recruited his now-wife, Kathy Long Maritato, PT.
Since then Kathy and Tony have grown Total Therapy Solutions LLC into a successful private practice with two locations in Ohio.
Tony spends his free time teaching other therapists how to contract with and bill Medicare for outpatient therapy services.
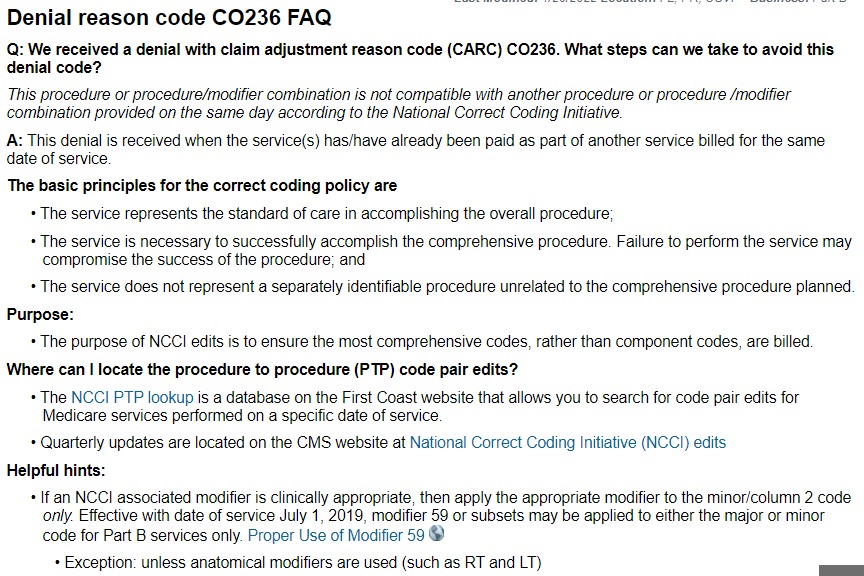
Denial reason code CO 236
Facebook Question About CO 236: "Hi All!Medicare denial received, paid all CPT except the Re-Eval We billed 97164, 97112, 97530, 97535 - they denied 97164 for CO 236 Any help on corrected billing to get this paid is appreciated!Thank you!" Medicare Physical Therapy...
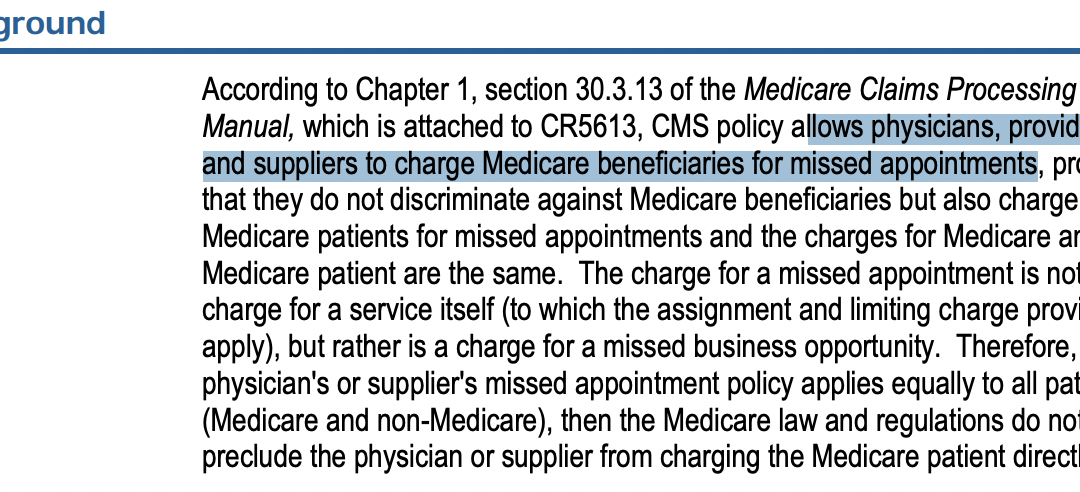
Cancellation No Show Policy Medicare
Cancellation No Show Policy Medicare Question: "Cancellation fee:Have any mobile therapists ever charged a full private pay rate for cancellation where you traveled to the Pt and they did not answer the door or charge that to a teletherapy client who did not "show"? I...
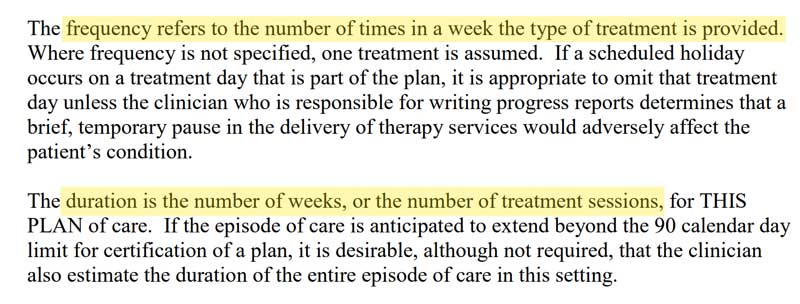
Occupational Therapy Medicare Plan of Care Frequency and Duration
Medicare Plan of Care Question about Occupational Therapy Medicare Plan of Care Frequency and Duration: "I am a mobile OP PT provider, have a potential patient who has Medicare as her primary. Can I write a PT POC for a specific number of visits over a certain time...
Does My PT Plan of Care Need to Say Outpatient In The Home?
Question: "For mobile PTs... When you are sending a POC to the Dr are you specifically writing outpatient PT in the patients home (or something similar specifying they are being treated in their house)? If I write that I don't want the Dr thinking home health. Also, I...
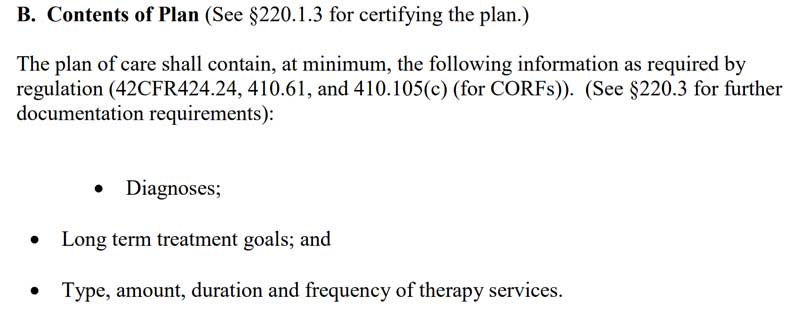
CPT Code Therex 97110
CPT Code Therex 97110 CPT Code Therex 97110 (Therapeutic Exercise) was the 4th highest ranked procedure code listed on the 2021 CMS CERT Overpayment Top 20 List.What is the Medicare definition of CPT Code Therex 97110? Reference: LCD L34049 "Therapeutic exercises are...
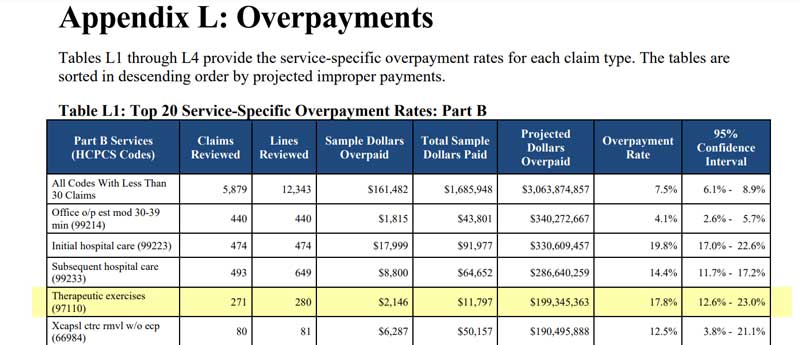
Medicare Provider Enrollment Rejection
Nothing is more frustrating than when you Medicare provider enrollment rejection notice arrives in your email inbox. What happens if your physical therapy Medicare provider enrollment application is denied? If you are a physical therapist applying to become a...

Does Medicare Cover Massage Therapy
Massage therapy is only a covered service for Medicare when it is provided as part of a comprehensive treatment. When providing massage only it is not a covered service and therefore providers are allowed to provide it to Medicare beneficiaries for cash pay (self pay) physical therapy.

Best Physical Therapy YouTube Channels in 2022
This article is a YouTube channel roundup of 2022's BEST Physical Therapy YouTube Channels. Selection Criteria... My Personal Opinion! This is a growing list. I will be adding channels as I find them. Check back regularly to see new listings.Physical Therapy YouTube...

CPT Code 97010 Does Insurance Pay for Ice Packs
Does Insurance Pay for CPT Code 97010 Technically, yes, UnitedHealthcare does pay for CPT code 97010, (Application of a modality to one or more areas; hot or cold packs). I say "technically" because it is paid as a bundled payment. Ice packs, moist heat, and other...

Good Faith Estimate and No Surprise Act for Physical Therapy in 2022
In this video interview with Nancy Beckley from https://nancybeckley.com/ d we discuss: Good Faith Estimate No Surprise Act Physical Therapy Billing Occupational Therapy Billing Medicare, Medicaid, Self Pay Services, and more. Highlights and Resources: 45 CFR...