What is a Medicare ABN Form?
According to the Medicare Claims Processing Manual Chapter 30 Section 50:
” The ABN is an Office of Management and Budget (OMB)-approved written notice issued by healthcare providers and suppliers for items and services provided under Medicare Part B. With the exception of DME suppliers, only healthcare providers and suppliers who are enrolled in Medicare can issue the ABN to beneficiaries.
The ABN is given to beneficiaries enrolled in the Medicare FFS program. It is not used for items or services provided under the Medicare Advantage (MA) Program or for prescription drugs provided under the Medicare Prescription Drug Program (Part D). Skilled Nursing Facilities (SNFs) issue the ABN for Part B services only.
The Skilled Nursing Facility Advance Beneficiary Notice of Non-coverage (SNF ABN), CMS Form 10055, is issued for Part A SNF items and services. Section 70 of this chapter contains information on SNFABN issuance.” – Link
Who Can Use a Medicare ABN Form?
Licensed physical therapists who are contracted with Medicare may use the Medicare ABN when delivering services that are no longer medically necessary and thereby no longer covered by Medicare.
Mandatory ABN
The most common use of the Medicare ABN is when a patient has been receiving physical therapy services and that patient has met his or her stated goals. Once the patient’s goals have been met and the therapist’s plan of care is complete, a continuation of therapy services may no longer be reasonable and medically necessary.
At this time a mandatory ABN may be issued if the patient chooses to continue to work with the therapist to achieve higher functional performance.
In this case, the patient is notified of the financial cost of the continued service, a mandatory ABN is completed following the instructions in CMS Chapter 30, and a single ABN is issued for the entire episode of continued service.
Another common use of the mandatory ABN is when a Medicare beneficiary has exceeded the financial threshold and the therapist has determined that continuation of therapy is no longer medically necessary.
Voluntary ABN (Optional ABN)
An optional ABN may be issued as a courtesy to the patient informing him of the financial obligations associated with the chosen service.
An option ABN may be utilized when the service is statutorily excluded or never covered by the Medicare benefit policy.
Examples of services that are never covered by Medicare may include personal training, golf performance, wellness, and generalized fitness.
* Note: When an optional ABN is issued, the client should not be asked to choose an option or sign the document.
How to Complete an ABN in Physical Therapy
Several resources exist with instructions from CMS and examples of completed mandatory ABN’s.
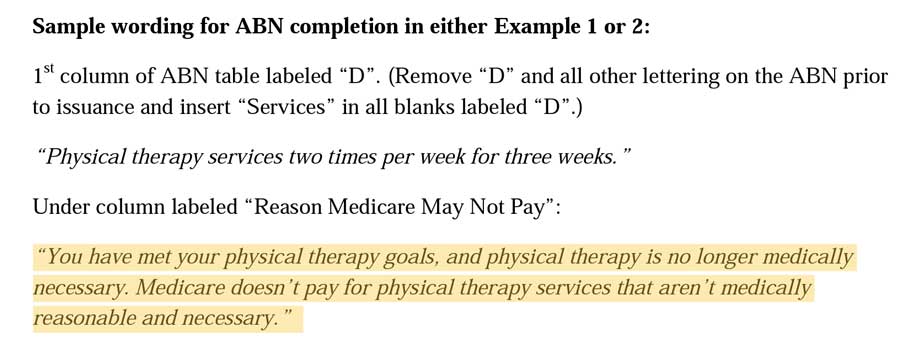
Below is a screenshot of an out-of-date resource that provides an excellent narrative used in the “Reason Medicare May Not Pay” section of the form.
Should a Cash-Based Physical Therapist Use A Medicare ABN Form?
No. If you have no contracted affiliation with Medicare then you are not eligible to utilize a Medicare ABN form.
The Medicare ABN form is only for physical therapists contracted with Medicare. The ABN is not a way for CashPTs to avoid the mandatory claim submission law associated with delivering Medicare-covered services to Medicare beneficiaries.
What Happens if I Issue an ABN and Medicare Pays the Claim?
Real Life Scenario – A therapist recently issued a mandatory ABN. His patient chose option 1 which required that the physical therapist submit the claim to Medicare. The physical therapist applied the correct GA modifier to the claim and fully expected Medicare to deny payment.
To his surprise, Medicare issued payment for the claim. Now this therapist was required to refund the payment to the patient and hope that Medicare doesn’t reverse this payment decision leaving the therapist with the responsibility of rebilling the physical therapy patient and explaining what happened.
Additional Resources and Links:
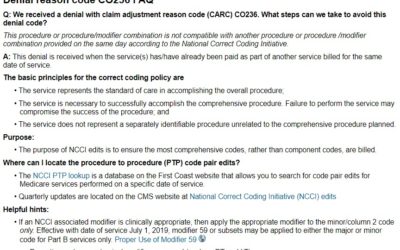
Denial reason code CO 236
Facebook Question About CO 236: "Hi All!Medicare denial received, paid all CPT except the Re-Eval We billed 97164, 97112, 97530, 97535 - they denied 97164 for CO 236 Any help on corrected billing to get this paid is appreciated!Thank you!" Medicare Physical Therapy...
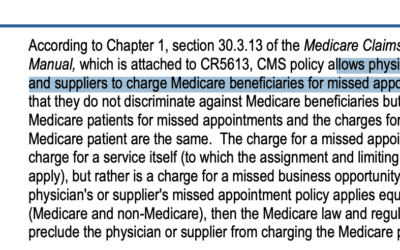
Cancellation No Show Policy Medicare
Cancellation No Show Policy Medicare Question: "Cancellation fee:Have any mobile therapists ever charged a full private pay rate for cancellation where you traveled to the Pt and they did not answer the door or charge that to a teletherapy client who did not "show"? I...