Can You Charge a No Show Fee to a Medicare Beneficiary?
Yes, you are allowed to charge a no show fee to a Medicare beneficiary as long as you have an established no show fee policy for all patients at your practice.
“According to Chapter 1, section 30.3.13 of the Medicare Claims Processing Manual – CMS’s policy is to allow physicians and suppliers to charge Medicare beneficiaries for missed appointments, provided that they do not discriminate against Medicare beneficiaries but also charge non-Medicare patients for missed appointments.”
Reference: Chapter 1, section 30.3.13 of the Medicare Claims Processing Manual
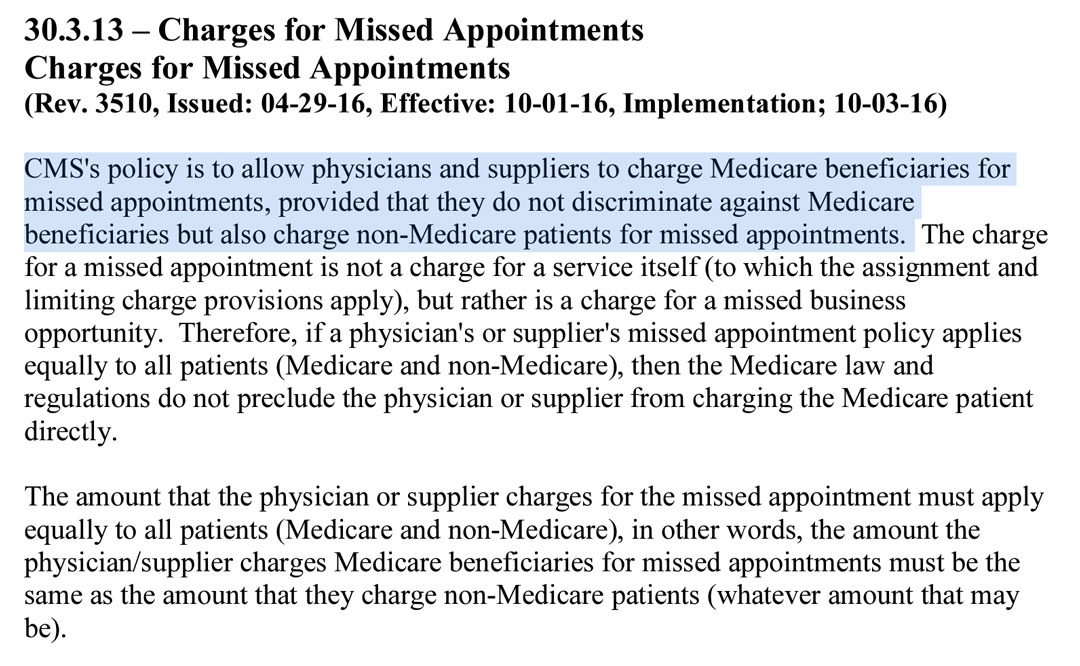
Missed Business Opportunity
This is an interesting choice of words. Since the fee is not for an actual covered service, the provider is not required to issue an advanced beneficiary notice and is not subject to the Medicare physician fee schedule.
What Qualifies as a Missed Appointment?
CMS Chapter 1, section 30.3.13 does not provide specific guidance in regards to how a missed appointment is defined.
No Shows
Your practice must have a policy manual and within that policy manual, you must define, in writing, what a “no show” is.
For example, a “no show” may be defined as a non-arrival within 5-minutes of the scheduled appointment time.
Why 5-minutes? Because some practices could have an established policy that states that once a patient is more than 5-minutes late for an appointment that appointment is considered a no-show and the scheduled therapist will perform other activities for the remainder of the appointment time.
Cancellations
Your cancellation policy must also describe the difference between a cancellation that may be rescheduled and a cancellation that is considered a missed appointment.
Many providers have chosen a 24-hour threshold to say that any cancellation occurring with less than 24-hours of notice is considered a missed appointment and subject to the missed appointment policy.
Weekend Cancellations?
How do you plan to handle weekend cancellations? There will be occasions in which your patient has an appointment scheduled for Monday morning and your 24-hour cancellation policy would require that patient to cancel on or before Sunday morning.
Voicemail Cancellations
Will your policy allow for voicemail cancellations? If your voicemail system timestamps the day and time a message is left you may want to include this in your cancellation policy.
Email Cancellations
Does your practice accept cancellations by email? Similar to voicemail, these may be acceptable to you if the email is timestamped with more than 24-hour notice, but this must be included in your policy manual.
Text Message Cancellations
My favorite method as a practice owner is text message cancellation. I may not want to check voicemail or email over the weekend, but if I receive a text message cancellation the first appointment on an otherwise busy morning I will usually appreciate the notification and use that time accordingly.
Your policy manual should indicate whether you accept text message cancellations and what telephone number that message should use.

Medicare Provider Enrollment Rejection
Nothing is more frustrating than when you Medicare provider enrollment rejection notice arrives in your email inbox. What happens if your physical therapy Medicare provider enrollment application is denied? If you are a physical therapist applying to become a...
Does Medicare Cover Massage Therapy
Massage therapy is only a covered service for Medicare when it is provided as part of a comprehensive treatment. When providing massage only it is not a covered service and therefore providers are allowed to provide it to Medicare beneficiaries for cash pay (self pay) physical therapy.
Best Physical Therapy YouTube Channels in 2022
This article is a YouTube channel roundup of 2022's BEST Physical Therapy YouTube Channels. Selection Criteria... My Personal Opinion! This is a growing list. I will be adding channels as I find them. Check back regularly to see new listings.Physical Therapy YouTube...
CPT Code 97010 Does Insurance Pay for Ice Packs
Does Insurance Pay for CPT Code 97010 Technically, yes, UnitedHealthcare does pay for CPT code 97010, (Application of a modality to one or more areas; hot or cold packs). I say "technically" because it is paid as a bundled payment. Ice packs, moist heat, and other...
Good Faith Estimate and No Surprise Act for Physical Therapy in 2022
In this video interview with Nancy Beckley from https://nancybeckley.com/ d we discuss: Good Faith Estimate No Surprise Act Physical Therapy Billing Occupational Therapy Billing Medicare, Medicaid, Self Pay Services, and more. Highlights and Resources: 45 CFR...