Yes, Medicare supplemental plans, also known as Medigap plans, do cover physical therapy services.
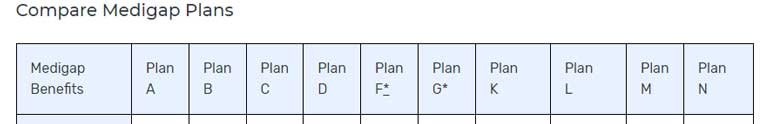
These plans are divided into plan names based on letters. Below is a screenshot from Medicare.gov showing the list of possible plans.
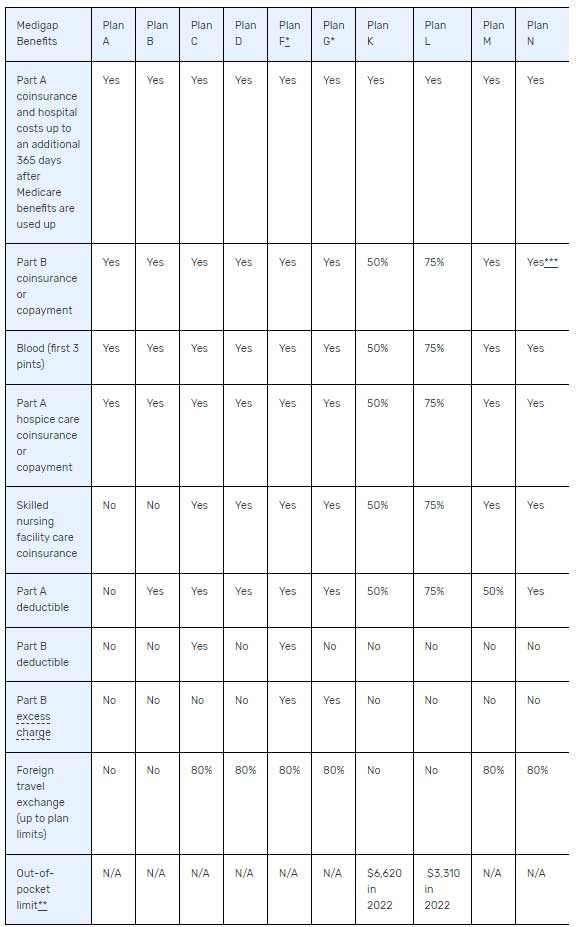
To see what each plan covers, Medicare.gov has also published this table.
Does a physical therapist who is contracted with Medicare Part B need to also contract with the Medicare supplemental plan provider?
No! If a physical therapist or occupational therapist is a contracted participating provider with Medicare Part B then the supplemental plan does not require you to also individual contract with them.
The supplemental plan will pay you, the provider, based on the Medicare allowed amount coinsurance and the particular plan’s coverage.
What is a non-supplemental secondary?
A non-supplemental secondary insurance plan could be a stand-alone policy from a spouse’s employer or a different kind of health insurance plan that is not a supplemental plan.
For example, if the patient is a Medicare part B beneficiary and has a spouse who is still employed and has an insurance plan through that employer. The spouse’s insurance coverage could act as a secondary to the patient’s Medicare part B coverage for physical therapy services.
In this case, the secondary plan is not a Medicare supplemental and is not required to pay if the provider is not contracted and the plan does not offer out-of-network coverage.
Other reasons a non-supplemental secondary insurance plan might not pay for physical therapy.
If the non-supplemental secondary insurance has its own patient cost share in the form of a deductible, copay, or co-insurance and the patient cost share is greater than the 20% Medicare part B coinsurance then the balance due would flow through the secondary plan to the patient and the patient would be responsible for payment.
How to identify a supplemental vs non-supplemental secondary insurance policy.
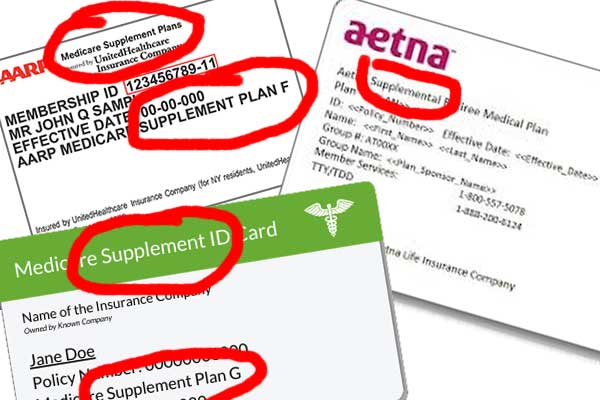
In some cases, the Medicare supplemental insurance card will say “supplemental” somewhere on the card. It might also have the plan name as in “Plan G” somewhere on the card.
Not all supplemental insurance cards will say supplemental, but if you call the provider relations number on the card to verify the coverage you will be able to confirm that it is or is not a supplemental.
Conclusion:
* Yes, Medicare supplemental plans will pay for physical therapy services even when the provider isn’t contracted with the plan payer.
* No, a non-supplemental secondary plan is not required to pay the Medicare Part B Coinsurance if the provider isn’t individually contracted with the plan payer.
Related articles:
3 Best Reactivation Strategies to Get Physical Therapy Patients Back in your Clinic
What is a Reactivation Strategy? Reactivation strategies are systems to help a physical therapy clinic stay in touch with discharged patients. Depending on your patient demographic, discharged patients will likely need your services again in the future. Developing a...
9 Best Physician Marketing Strategies for a Mobile Physical Therapy Practice in 2022
Best Physician Marketing Strategies for Physical Therapists As a mobile physical therapist in private practice, you have two major obstacles to overcome. Nobody knows that you exist. Most people will assume you are a Medicare Part A home health company. Developing...
9 Ways To Keep Physical Therapy Patients Motivated
What exactly is 'physical therapy motivation' and how can it help improve patient compliance and outcomes? First, let's define motivation: mo·ti·va·tion /ˌmōdəˈvāSH(ə)n/ noun 1. the reason or reasons one has for acting or behaving in a particular way. "escape can be a...

Anthony Maritato, PT
Physical Therapy / Private Practice Owner
Being a licensed physical therapist has always been a passion of mine. The best way I have found to protect that passion is by creating AMAZING cash-generating money machines that provide financial security and freedom thereby allowing me to continue treating patients for the joy of treating patients.