If I asked 100 licensed physical therapists what they hate most about their job 100 of them would list documentation in the top 3.
Physical Therapy Documentation Templates are an important way to reduce documentation time, headaches, and mistakes.
In this article, I will share some of the best physical therapy documentation templates available for FREE and some premium templates available for purchase.
What are Physical Therapy Documentation Templates
Physical therapy documentation templates are simply a predetermined structure designed to reduce errors, increase efficiency, and improve job satisfaction.
A template might be as simple as an outline to help guide a clinician’s initial evaluation or it might be as complex as a complete evaluation with blanks left for new information.
Is using a template the same as cutting and pasting?
No! Templates predate EMRs. We used to use paper forms before EMRs to help guide our physical therapy documentation. Those forms were templates. Now with technology, more of the form might auto-populate. For example, a template that auto-populates the date may save some time. A template that auto-date stamps the document when the clinician signs and closes the document may help compliance.
Templates are great time savers.
The challenge in today’s environment is finding templates you LOVE and use.
Physical Therapy SOAP Note Example
What does SOAP Note mean?
- S: Subjective – this is the part of the note that documents what the patient says, feels, or believes. Example: How are you feeling today? or How did you feel after your last treatment?
- O: Objective – this is the measurable part of the note. An objective measure might be 10 repetitions of an exercise or the distance in meters your patient walked.
- A: Assessment – This portion of the note requires the clinician’s professional judgment and interpretation of clinical findings. “Based on my assessment, Mrs. Patient is unsafe to return to work and will require 8 more physical therapy treatments.”
- P: Plan – This portion of the note includes what will be changed or performed next visit. It could also include information needed for discharge. “Mrs. Patient will perform her home exercise program for 2 weeks before returning to my offer to start the next phase of her treatment plan.”
SOAP notes are commonly used in outpatient physical therapy services for daily treatment notes. Under Medicare Benefit Policy Manual guidelines, if a treatment note contains all of the progress report’s required elements then a separate progress report is not required.
* Note: Although a separate progress report may not be required it is often still recommended.
Recommended Treatment Note Templates
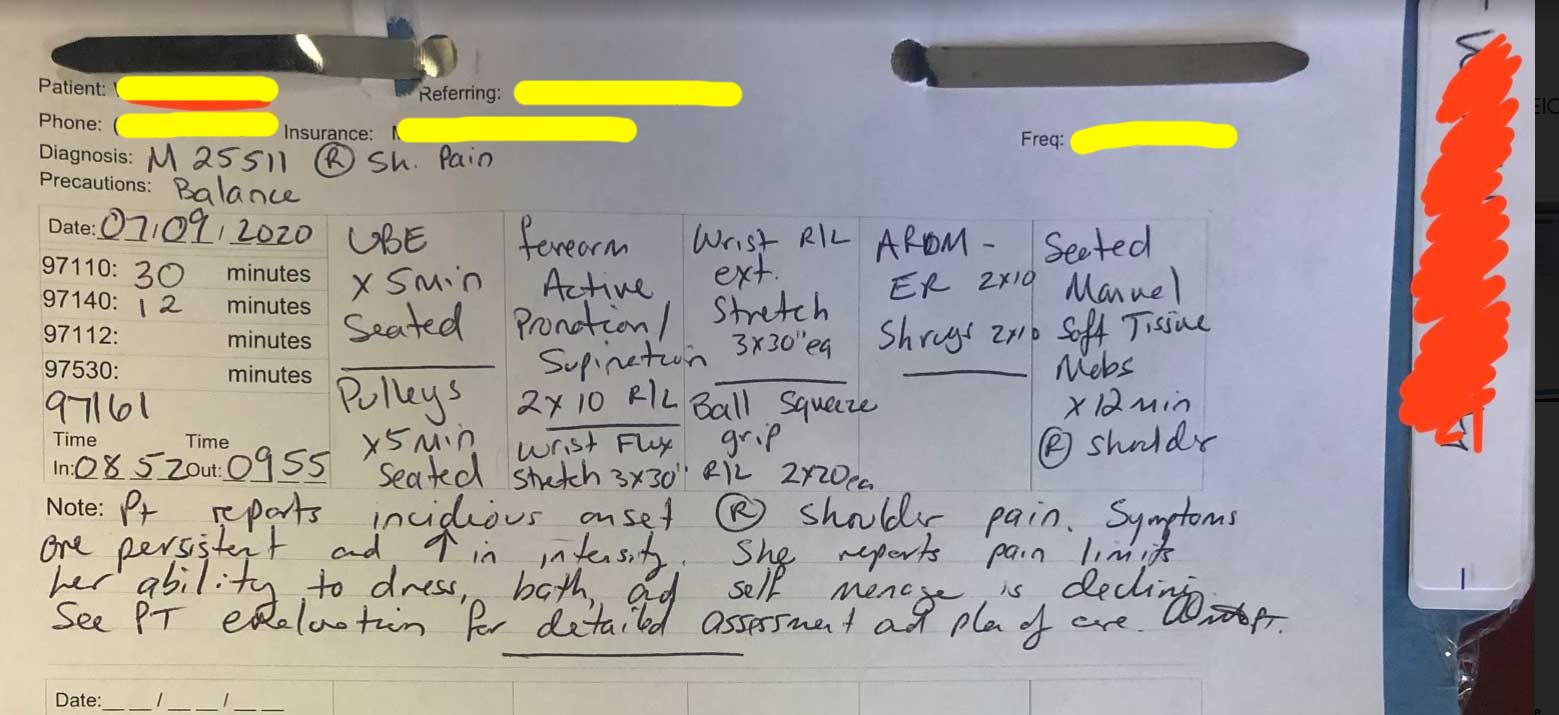
PTProgress > Sample Treatment Note Template
Where Can I Buy Physical Therapy Forms
- Tim Fratecelli from PTProgress.com has created some really great, low-cost templates.
- Max Shippen from Unsubscribed Healthcare has a phenomenal template.
Physical Therapy Documentation Cheat Sheet
If you have not already created a physical therapy documentation cheat sheet then you should. Each third-party payer will have different fundamental requirements. Creating a template and cheat sheet for each payer can save you a boatload of time and headaches down the road.
I am working on some cheat sheets for Medicare, United Healthcare, and other third-party payers. Once I finish them I will share them here.
Physical Therapy Evaluation Templates
What is the difference between an evaluation template and a plan of care template?
Medicare benefit policy manual guidelines state that a physical therapy evaluation and plan of care may be two documents or one combined document. Each document has required elements and if all required elements are on one document there is no need for separate documents.
Here is a sample physical therapy evaluation template from Lancaster Ortho.
Here is a sample physical therapy evaluation and re-evaluation form from Kissner.net
Physical Therapy Progress Report Templates
Be ready to have your mind blown!
Below is a screenshot taken from the Medicare Benefit Policy Manual page 195. The highlighted area is a sample progress report written for a patient receiving speech-language pathology. This report covers up to 10 treatment visits and spans 26 calendar days.
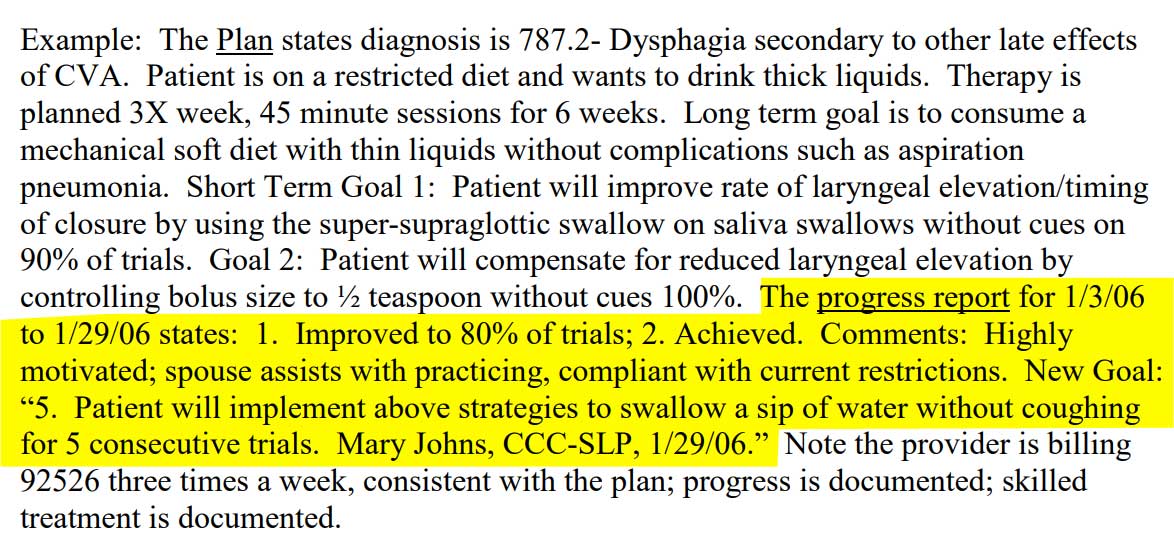
Have you ever written a 10 visit progress report so succinctly? I know I have not. But if you follow the Medicare published guidelines, every required element of a progress report is contained within the example and a couple of bonus elements are included.
Physical Therapy Treatment Note Templates
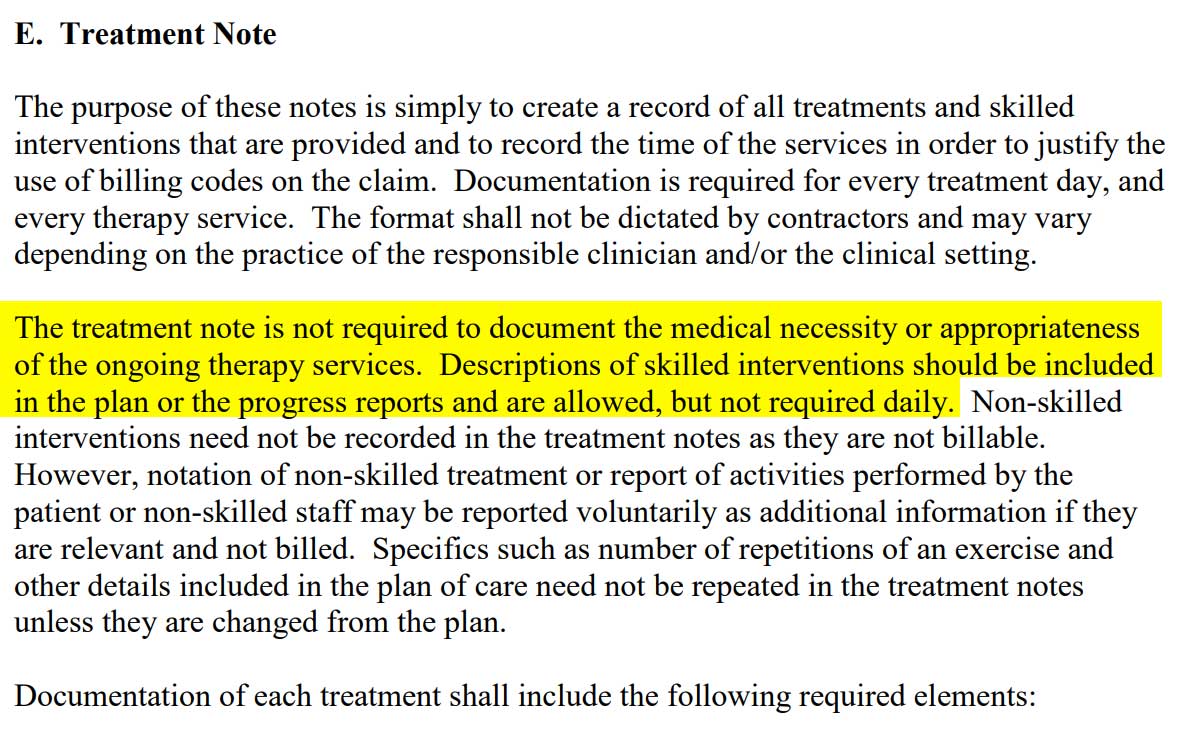
Another revelation related to Medicare’s documentation requirements.
“The treatment note is not required to document the medical necessity or appropriateness of the ongoing therapy services.”
I can’t tell you how many hours, days, and weeks of my life have been spent trying to document medical necessity in every daily treatment note to ensure payment.
Physical Therapy Documentation Resources and Publications
Start with your state practice act guidelines on physical therapy documentation. Next, find resources published by third-party payers. For example, CMS and local Medicare MACs will publish NCD, LCD, and articles.
Professional organization position papers may offer additional guidance and textbook publications.
Does Medicare Supplemental Insurance Cover Physical Therapy
Yes, Medicare supplemental plans, also known as Medigap plans, do cover physical therapy services. These plans are divided into plan names based on letters. Below is a screenshot from Medicare.gov showing the list of possible plans.To see what each plan covers,...
How to Create a Physical Therapy Referral Pad
Creating a physical therapy referral pad to market your physical therapy business is easy. Thankfully, physical therapy is not a controlled substance so there are no real hard and fast rules around creating these referral pads. In this article, I will share my best...
BEST Affiliate Marketing for Physical Therapists
Affiliate Marketing for Physical Therapists in Private Practice If you are like me, you hate the thought of feeling pressured to keep a patient in the clinic 3 more minutes so you can charge 1 more unit. You hate the feeling of threatening patients with cancelation...
What is a Letter of Medical Necessity?
A letter of medical necessity is simply a document supporting the need for a prescribed assistive device that may be used by the patient to improve or treat a medical condition. If a physical therapist determines a patient may require a walker to assist in...
3 EASY Ways To Make More Money As A Physical Therapist in 2022
1.) Selling Info-Products and Digital Courses Informational Graphics Creating and selling info-graphics and downloadable pdfs is a great way to earn extra income as a physical therapist. The easiest way to get started is to use software like Canva to search templates....