CashPT for Medicare Beneficiaries Who Want Something Better
Mandatory Claim Submission Law
40.33 – Mandatory Claims Submission (Rev. 222, Issued: 05-13-16, Effective: 08-15-16, Implementation; 08-15-16) Section 1848(g)(4) of the Act, “Physician/Practitioner Submission of Claims,” regarding mandatory claims submission, does not apply once a physician or practitioner signs and submits an affidavit to the Medicare contractor opting out of the Medicare program, for the duration of the physician’s or practitioner’s opt-out period, unless the physician or practitioner knowingly and willfully violates a term of the affidavit.
Other Non-Covered Medicare Services for CashPTs
- Anything related to recreation and sports.
- Services that have been deemed as not medically necessary by the patient’s physician.
- Services rendered in a location other than the patient’s home or your clinic.
- Services delivered by asynchronous electronic communication such as email or text messaging.
- Asynchronous video programming.
- Some versions of home exercise programs.
- Services delivered by someone other than a licensed therapist or assistant working under the direct supervision of a therapist.
Build Your Provider Network
If I were still in the cashPT only business model I would network with other Medicare contracted providers to build my provider network.
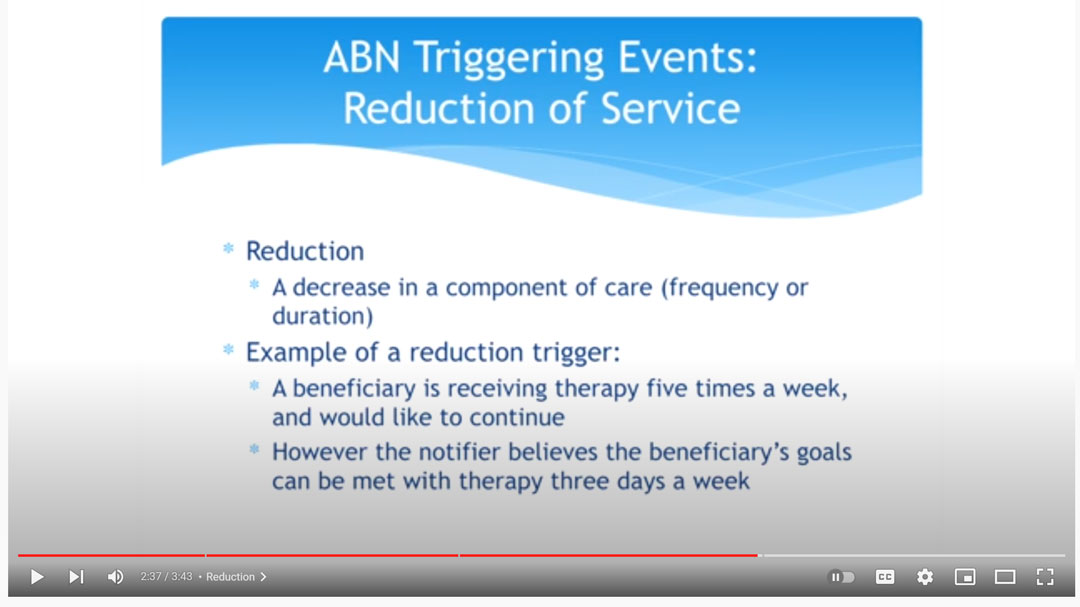
In this video, NGSMedicare MAC explains how when a patient wants 5 days a week of physical therapy services, but only 2 days a week is medically necessary, the patient may choose to self pay for the additional three days a week.
In this case, an ABN would be issued by the contracted provider if the contracted provider is supplying the additional 3 days a week of treatment.
If the extra treatments are provided by an unaffiliated physical therapist no ABN is issued.
Can a CashPT use an ABN?
No. Only Medicare contracted participating and non-participating providers may use a CMS Advance Beneficiary Notice (ABN).
Medicare Advantage
Does the ABN apply to Medicare Advantage plans?
No. The ABN is not applicable to Medicare Advantage insurance plans. Keep in mind that the Mandatory claim submission law does not apply to Medicare Advantage plans. Physical therapists that are not affiliated with Medicare Part B in any way are allowed to treat patients with Medicare Advantage insurance.
Can a Contracted Medicare Provider Offer CashPT?
Yes! The best of both worlds is to become a contracted Medicare provider who offers both Medicare covered and non-covered services.
For example, Medicare does not cover dry needling CPT Code 20560 and CPT Code 20561 when delivered by a licensed physical therapist. If you are a contracted Medicare provider your initial physical therapy evaluation would be a covered service, then if you determined that dry needling would benefit your patient and you are capable of delivering the dry needling intervention you would be allowed to charge a self pay rate for the dry needling intervention.
Medicare Covered Initial Evaluation and Dry Needling CashPT
In this case, Medicare would reimburse the Medicare allowed amount for the physical therapy evaluation CPT Code 97161 – $98 and you would charge the patient your standard CashPT rate for CPT Code 20560 – $60.
The total revenue for a 30-minute session would be $158.
Both of these services may be provided in the same day. You may choose to supply an optional ABN as a courtesy to your patient, but it is not required.
Summary:
- The federal mandatory claim submission law requires all healthcare providers to submit claims for service to Medicare when providing Medicare-covered services.
- If you are a cashpt with no affiliation to Medicare Part B and you want to help Medicare beneficiaries an easy way to accomplish this is to work with a contracted Medicare provider.
- If you become a contracted Medicare provider you would be allowed to provide both covered and non-covered services.
Read more:
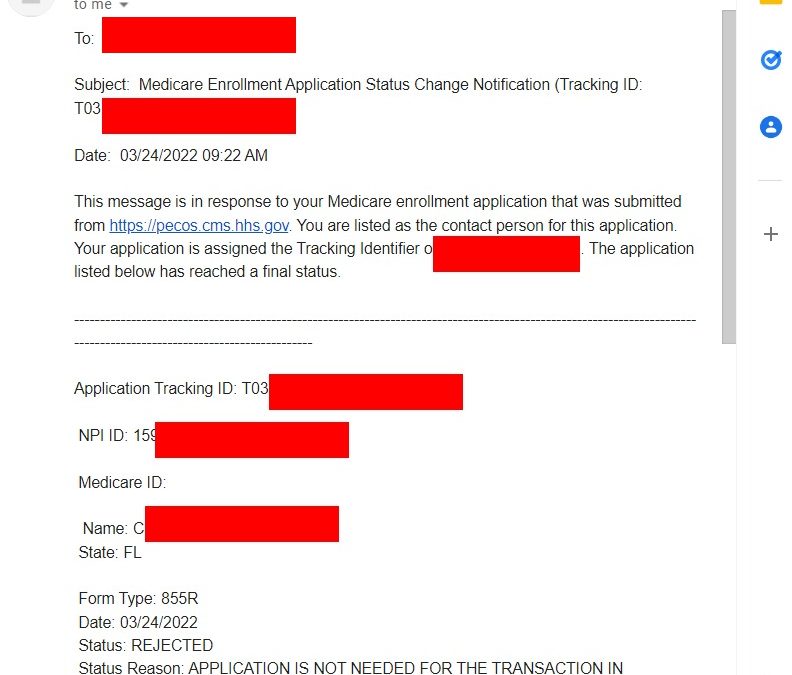
Medicare Provider Enrollment Rejection
Nothing is more frustrating than when you Medicare provider enrollment rejection notice arrives in your email inbox. What happens if your physical therapy Medicare provider enrollment application is denied? If you are a physical therapist applying to become a contracted...

Does Medicare Cover Massage Therapy
Massage therapy is only a covered service for Medicare when it is provided as part of a comprehensive treatment. When providing massage only it is not a covered service and therefore providers are allowed to provide it to Medicare beneficiaries for cash pay (self pay) physical therapy.

Best Physical Therapy YouTube Channels in 2022
This article is a YouTube channel roundup of 2022's BEST Physical Therapy YouTube Channels. Selection Criteria... My Personal Opinion! This is a growing list. I will be adding channels as I find them. Check back regularly to see new listings.Physical Therapy YouTube...

CPT Code 97010 Does Insurance Pay for Ice Packs
Does Insurance Pay for CPT Code 97010 Technically, yes, UnitedHealthcare does pay for CPT code 97010, (Application of a modality to one or more areas; hot or cold packs). I say "technically" because it is paid as a bundled payment. Ice packs, moist heat, and other similar...

Good Faith Estimate and No Surprise Act for Physical Therapy in 2022
In this video interview with Nancy Beckley from https://nancybeckley.com/ d we discuss: Good Faith Estimate No Surprise Act Physical Therapy Billing Occupational Therapy Billing Medicare, Medicaid, Self Pay Services, and more. Highlights and Resources: 45 CFR 149.610(b)...