How much does Medicare pay for physical therapy
This article will specifically reference the Medicare Part B Physician Fee Schedule look-up tool to determine how much does Medicare pay for physical therapy.
Medicare Part B payment rates for a physical therapy initial evaluation CPT code 97161?
Medicare Part B has reduced physical therapy rates from $98.01 in 2021 to $95.13 in 2023. This change is specifically for outpatient physical therapy reimbursement in the state of Ohio.
To determine Medicare Part B reimbursement allowed amounts for the calendar year and geographic location you will need to either go to your local MAC website and search their physician fee schedule, or you can find the same information on the CMS website under Physician Fee Schedule Look-Up Tool.
Below is a table showing Medicare Part B allowed amounts for participating providers in Ohio.
Medicare allowed amount by CPT Code: 97110, 97530, and 97140?
Below is a table containing the CMS Physician Fee Schedule allowed amounts for participating physical therapy providers. This table compares reimbursement rates between 2023 and 2021 for Ohio’s CGS Medicare.
Reimbursement will vary by state so it is important that you choose your specific MAC or location.
You can see that the Medicare Part B participating provider allowed amounts are as follows:
| CPT Code | 2023 Payment | 2021 Payment |
| 97110 | $27.89 | $29.21 |
| 97112 | $31.96 | $33.82 |
| 97140 | $25.72 | $26.92 |
| 97161 | $95.13 | $98.01 |
| 97530 | $34.80 | $37.46 |
What is the difference between Facility and Non-Facility Price?
Physical therapists, occupational therapists, and speech-language pathologists in private practice use the Non-facility price to estimate the allowed amount.
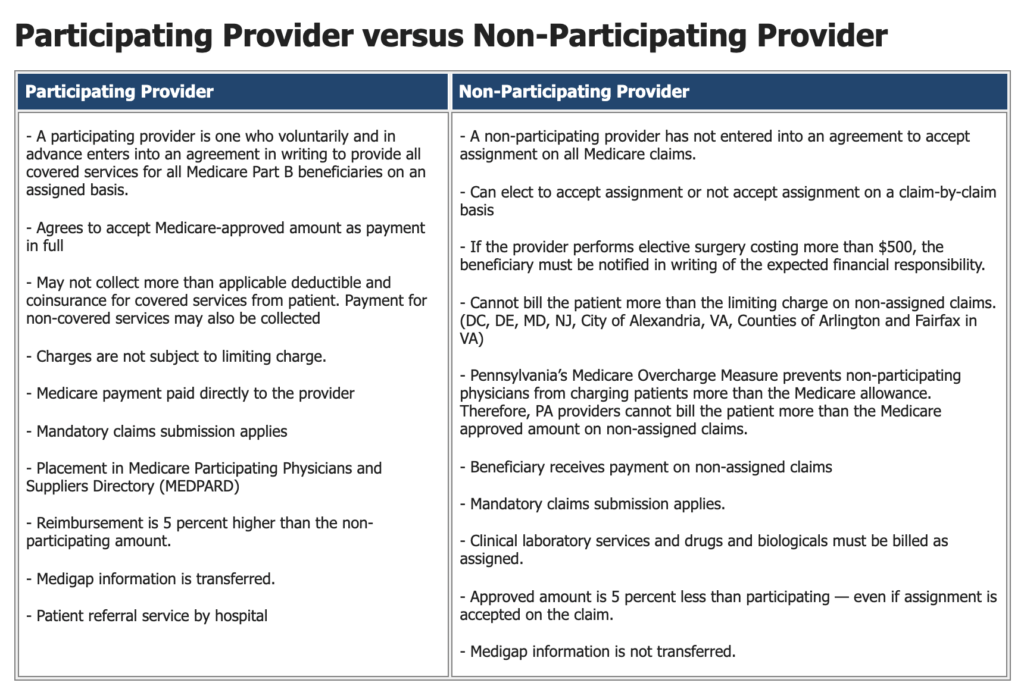
What is the difference between PAR and NonPAR allowed amounts?
The NonPAR allowed amount is 95% of the PAR allowed amount.
* Source: Novitas-Solutions
Is it better for a physical therapist to be PAR or NonPAR?
In my opinion, it is NOT better for a physical therapist, occupational therapist, or speech-language pathologist to be Non-PAR (non-participating).
In the following video, I will share the reasons why Non-PAR is not better, but to summarize it here I have created a list:
- Both participating and non-participating providers are required to comply with all of the same Medicare regulations.
- Both participating and non-participating providers are required to submit claims on behalf of the beneficiary for covered services, but Non-PAR claims are not automatically forwarded to the patient’s supplemental insurance.
- Yes, it is true the Non-PAR provider may choose not to accept assignment and charge the Medicare beneficiary up to 115% of the Non-PAR fee schedule, but the Non-PAR fee schedule is lower and the provider must collect from the patient either at the time of service or after. This results in increased administrative costs.
- If a single Medicare beneficiary chooses not to pay a Non-PAR provider then the cost of collections and other measures may eliminate the potential small increase in reimbursement.
Does Medicare Part B have a CAP on Physical Therapy Services?
No, Medicare Part B no longer has a cap. Now it is referred to as a financial threshold. Click here for information directly from CMS.
In 2023 the Medicare financial threshold for occupational therapy services is $2,230.
The Medicare financial threshold for physical therapy and speech-language pathology combined is $2,230.
What happens if physical therapy services exceed the financial threshold?
If therapy services continue to be medically necessary based on established CMS guidelines, local MAC published guidelines, and the clinical judgement of the provider, then the KX modifier may be added to the CPT code claim line item and payment will be issued from Medicare.
If therapy services are deemed no longer medically necessary AND the patient wants to continue to receive therapy services while paying out of pocket then the provider may choose to issue a mandatory advanced beneficiary notice (ABN) before continuing care.
What if a Medicare beneficiary does not have a secondary insurance plan?
If the Medicare beneficiary does not have a secondary insurance policy that Medicare part B will cover 80% of the allowed amount and the patient will be responsible to pay the remaining 20%.
The best practice for the physical therapist in this situation is to estimate the 20% coinsurance and collect that amount from the patient at the time of service.
After Medicare has processed the claims the physical therapist may review the Medicare determined 20% patient responsibility and either refund the patient if more than expected was collected or invoice the patient if a remaining balance exists.
Does a Medicare secondary insurance plan pay for out-of-network physical therapy?
A traditional Medicare supplemental plan in the secondary position will pay therapists contracted with Medicare just the same as if the therapist was contracted with the supplemental payer.
But non-supplemental secondary insurance plans are not required to pay non-contracted therapists. Each plan is different so you will need to verify coverage and determine any patient responsibility before delivering treatment.
How can I learn more?
The first Tuesday of each month I start a new LIVE cohort of students in my Zero to Paid Medicare Billing Course. For more information on the course visit this website’s homepage.
Additional and Related Article Links:
- How to apply for a Type 2 NPI
- How to INCREASE the Average Physical Therapist Salary
- 5 Best Books For Starting A New Physical Therapy Practice in 2021

Anthony Maritato, PT
Physical Therapist / Private Practice Owner
As a serial entrepreneur since the age of 7, Anthony (Tony) Maritato didn’t start his first physical therapy clinic until he was 26.
After recently graduating from Pennsylvania State University with a bachelor’s degree in Kinesiology, Tony fell in love with the profession of physical therapy. Not wanting to wait until getting his degree in Physical Therapy, Tony quickly opened a personal training studio which transitioned to a full-time physical therapy clinic once he recruited his now-wife, Kathy Long Maritato, PT.
Since then Kathy and Tony have grown Total Therapy Solutions LLC into a successful private practice with two locations in Ohio.
Tony spends his free time teaching other therapists how to contract with and bill Medicare for outpatient therapy services.
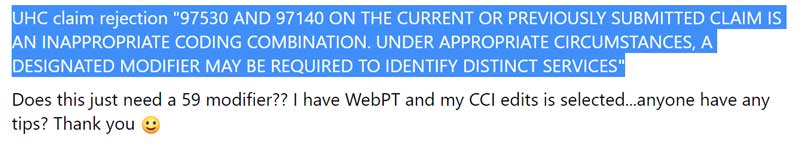
United Healthcare Requires 59 Modifier for CPT Code 97530 and CPT Code 97140 Combo
News 2022: Unitedhealthcare Requires 59 Modifier for Therapy Services Despite the recent changes to the NCCI edits no longer requiring CPT Code 97530 to require a 59 modifier when billed on the same date of service and by the same therapist as CPT Code 97140 some...
Physical Therapy Business Checks for Medicare PECOS
It may seem a little crazy, but YES, in 2022 Medicare still expects new business owners to have paper business checks. If you are submitting your Medicare provider enrollment via PECOS you are asked to either upload a copy of a voided business check or a letter from...
CashPT for Medicare Beneficiaries as After Care
CashPT for Medicare Beneficiaries Who Want Something Better This is a copy/paste of a post I shared on Facebook on September 9, 2022: "Medicare (and many other 3rd party payers) still pay the same rate for 97161, 97162, and 97163. ... I love simple cases. Easy fixes...
Physical Therapy Walk-In Evaluations
The following is a Facebook post from 09/07/2022 ... We all know how much we LOVE to people-watch....Airports, coffee shops, malls. We see every idiosyncrasy....Why then do we think every initial evaluation... even the easy ones, requires 60 minutes and multiple...
Medicare Definition of a Treatment Day Outpatient Physical Therapy
Medicare's Definition of a Treatment Day Medicare defines a treatment day as a single calendar day. A physical therapist might deliver multiple treatment sessions in a single treatment day. For the purposes of physical therapy progress reports, Medicare Part B...

Can a physical therapist bill Medicare for a progress note?
Can a physical therapist bill Medicare for a progress report or discharge summary? No, a physical therapist can not bill Medicare for a progress note. It is important you realize a progress note is not a physical therapy reevaluation. A progress report is not a...
PT School: (5) Great Reasons NOT to Go and (1) Reason to Go
1. The Crushing Debt No surprise here, the debt associated with PT school is crushing the life out of many new graduate DPTs. The Student Loan Planner website published that the average physical therapist debt is approximately $96,000. A 2020 APTA article suggests...

Medicare physical therapy cap 2022
What is the Medicare therapy threshold (formerly the therapy cap) for physical therapy in 2022? The 2022 Medicare therapy financial threshold for physical therapy is $2,150. Keep in mind that services delivered for speech-language pathology in the same calendar year...
5 Best Side Hustles for Physical Therapists in 2022
Side Hustles for Physical Therapists in 2022 These are 5 simple side hustles for physical therapists that may be used to either supplement your full-time income or replace your full-time income. Every physical therapist should have a side hustle! As a physical...
Best Physical Therapist Job Offer Templates for 2022
Before you accept any job as a physical therapist you should carefully review the physical therapist job offer letter. In this article, I will share what a physical therapist job offer letter template should include and what questions it should answer to protect both...