CashPT for Medicare Beneficiaries Who Want Something Better
Mandatory Claim Submission Law
40.33 – Mandatory Claims Submission (Rev. 222, Issued: 05-13-16, Effective: 08-15-16, Implementation; 08-15-16) Section 1848(g)(4) of the Act, “Physician/Practitioner Submission of Claims,” regarding mandatory claims submission, does not apply once a physician or practitioner signs and submits an affidavit to the Medicare contractor opting out of the Medicare program, for the duration of the physician’s or practitioner’s opt-out period, unless the physician or practitioner knowingly and willfully violates a term of the affidavit.
Other Non-Covered Medicare Services for CashPTs
- Anything related to recreation and sports.
- Services that have been deemed as not medically necessary by the patient’s physician.
- Services rendered in a location other than the patient’s home or your clinic.
- Services delivered by asynchronous electronic communication such as email or text messaging.
- Asynchronous video programming.
- Some versions of home exercise programs.
- Services delivered by someone other than a licensed therapist or assistant working under the direct supervision of a therapist.
Build Your Provider Network
If I were still in the cashPT only business model I would network with other Medicare contracted providers to build my provider network.
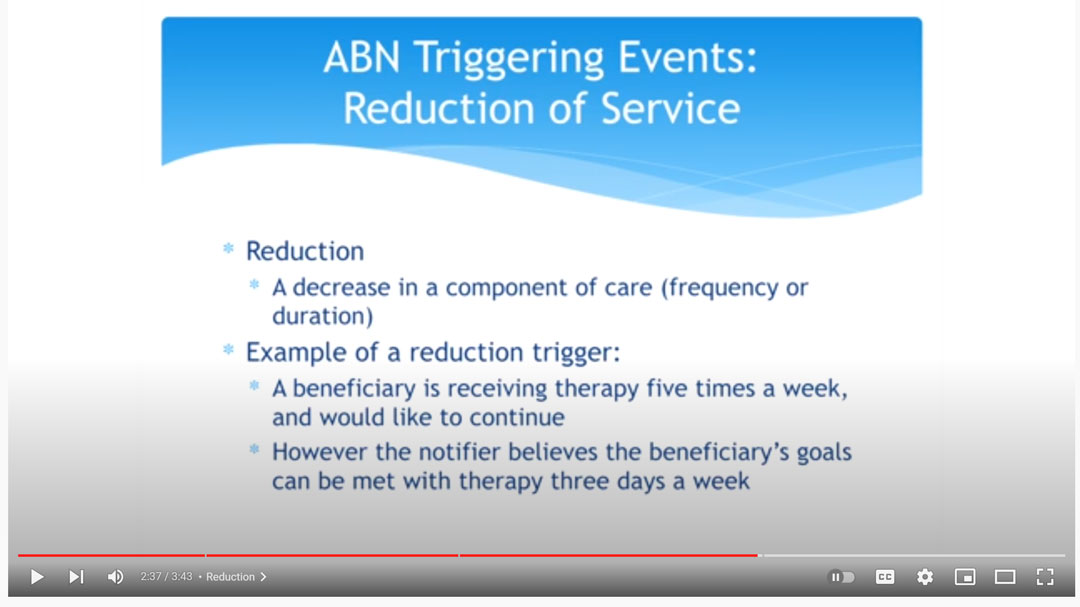
In this video, NGSMedicare MAC explains how when a patient wants 5 days a week of physical therapy services, but only 2 days a week is medically necessary, the patient may choose to self pay for the additional three days a week.
In this case, an ABN would be issued by the contracted provider if the contracted provider is supplying the additional 3 days a week of treatment.
If the extra treatments are provided by an unaffiliated physical therapist no ABN is issued.
Can a CashPT use an ABN?
No. Only Medicare contracted participating and non-participating providers may use a CMS Advance Beneficiary Notice (ABN).
Medicare Advantage
Does the ABN apply to Medicare Advantage plans?
No. The ABN is not applicable to Medicare Advantage insurance plans. Keep in mind that the Mandatory claim submission law does not apply to Medicare Advantage plans. Physical therapists that are not affiliated with Medicare Part B in any way are allowed to treat patients with Medicare Advantage insurance.
Can a Contracted Medicare Provider Offer CashPT?
Yes! The best of both worlds is to become a contracted Medicare provider who offers both Medicare covered and non-covered services.
For example, Medicare does not cover dry needling CPT Code 20560 and CPT Code 20561 when delivered by a licensed physical therapist. If you are a contracted Medicare provider your initial physical therapy evaluation would be a covered service, then if you determined that dry needling would benefit your patient and you are capable of delivering the dry needling intervention you would be allowed to charge a self pay rate for the dry needling intervention.
Medicare Covered Initial Evaluation and Dry Needling CashPT
In this case, Medicare would reimburse the Medicare allowed amount for the physical therapy evaluation CPT Code 97161 – $98 and you would charge the patient your standard CashPT rate for CPT Code 20560 – $60.
The total revenue for a 30-minute session would be $158.
Both of these services may be provided in the same day. You may choose to supply an optional ABN as a courtesy to your patient, but it is not required.
Summary:
- The federal mandatory claim submission law requires all healthcare providers to submit claims for service to Medicare when providing Medicare-covered services.
- If you are a cashpt with no affiliation to Medicare Part B and you want to help Medicare beneficiaries an easy way to accomplish this is to work with a contracted Medicare provider.
- If you become a contracted Medicare provider you would be allowed to provide both covered and non-covered services.
Read more:

Physical Therapist Vacation Coverage | CMS Locum Tenens Guidelines 2022
Physical Therapist Vacation Coverage Options? There are 2 primary options that exist for a private practice physical therapy clinic to hire an outside physical therapist to treat Medicare beneficiaries while another physical therapist is on vacation, maternity leave, or...
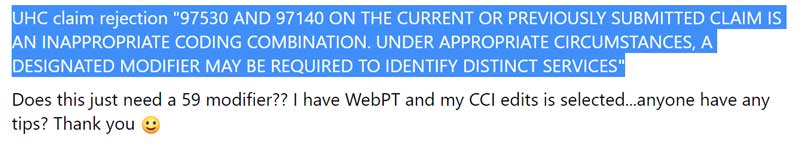
United Healthcare Requires 59 Modifier for CPT Code 97530 and CPT Code 97140 Combo
News 2022: Unitedhealthcare Requires 59 Modifier for Therapy Services Despite the recent changes to the NCCI edits no longer requiring CPT Code 97530 to require a 59 modifier when billed on the same date of service and by the same therapist as CPT Code 97140 some...
Physical Therapy Business Checks for Medicare PECOS
It may seem a little crazy, but YES, in 2022 Medicare still expects new business owners to have paper business checks. If you are submitting your Medicare provider enrollment via PECOS you are asked to either upload a copy of a voided business check or a letter from your...
Physical Therapy Walk-In Evaluations
The following is a Facebook post from 09/07/2022 ... We all know how much we LOVE to people-watch....Airports, coffee shops, malls. We see every idiosyncrasy....Why then do we think every initial evaluation... even the easy ones, requires 60 minutes and multiple layers of...
Medicare Definition of a Treatment Day Outpatient Physical Therapy
Medicare's Definition of a Treatment Day Medicare defines a treatment day as a single calendar day. A physical therapist might deliver multiple treatment sessions in a single treatment day. For the purposes of physical therapy progress reports, Medicare Part B requires a...